- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
ASCRS Updated guidelines on Management of Hemorrhoids
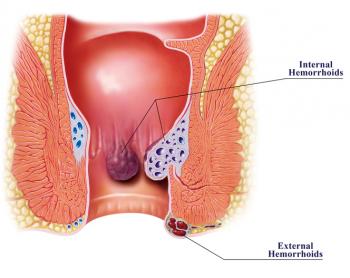
The American Society of Colon and Rectal Surgeons has released its updated guidelines on the management of hemorrhoids. The recommendations are published in Diseases of the Colon & Rectum.Hemorrhoids are among the most common problems encountered in today's world. The cardinal signs of internal hemorrhoids are hemorrhoid-pattern bleeding which is defined as painless bleeding with bowel movements and intermittent, reducible protrusion. The loosely related condition called thrombosed external hemorrhoid involves a clot in a vein under the anoderm that is the skin of the anal verge.
For hemorrhoids the first-line therapy involves
- Dietary modification promoting adequate fluids and fiber and counseling on defecation habits.
- In addition to this, phlebotonics offer "decent potential for relief."
- Patients with grade I–II (and some with grade III) internal hemorrhoidal disease can be treated with office-based procedures; the most effective is usually hemorrhoid banding.
Main Recommendations :
- A disease-specific history and physical examination should be performed, emphasizing degree and duration of symptoms and risk factors .
- Complete endoscopic evaluation of the colon is indicated in select patients with symptomatic hemorrhoids and rectal bleeding .
- Dietary modification consisting of adequate fluid and fiber intake and counseling regarding defecation habits typically form the primary first-line therapy for patients with symptomatic hemorrhoid disease.
- Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation (IRC). All office-based procedures attempt to reduce redundancy, reduce vascularity, and increase fixation of the anal cushion to its underlying muscle.Hemorrhoid banding is typically the most effective option.
- Rubber Band Ligation is a popular and effective treatment which is superior to sclerotherapy and IRC. In this procedure ligation of the hemorrhoidal tissue results in ischemia and necrosis of the prolapsing mucosa followed by scar fixation to the rectal wall.Ligation can be accomplished through a rigid anoscope or using a retroflexed flexible endoscope with a ligation attachment. Banding is less effective, less painful, and had fewer complications than surgery.
- Sclerotherapy involves the injection of a sclerosant into the apex of an internal hemorrhoid. It is successful in treating 75–90% of patients with first- to third-degree hemorrhoids.The sclerosing agents like 5% phenol in almond or vegetable oil or sodium tetradecyl sulfate are injected in to the submucosa at the apex of a hemorrhoidal bundle which leads to fibrosis of the submucosa with subsequent fixation of the hemorrhoidal tissue.The procedure is apt for treating grade I to III internal hemorrhoids.
- Infrared Coagulation involves the contact application of infrared radiation, essentially cauterizing hemorrhoid.It is most commonly used for grade I and II hemorrhoids and recent evidence has demonstrated that it is as efficacious as Rubber Band Ligation.
- Office-Based Procedures Are generally safe and Sepsis is a known complications.Because of the risk of significant bleeding, office procedures should generally be avoided in patients with thrombocytopenia or on warfarin, heparin products, and antiplatelet agents such as clopidogrel.
5.Surgical operations (hemorrhoidectomy, stapled hemorrhoidopexy, and Doppler-assisted hemorrhoidal artery ligation) is the treatment of choice in those patients who are refractory to or cannot tolerate office procedures,who have large, symptomatic external tags along with their hemorrhoids, who have large third-degree hemorrhoids, or who have fourth-degree hemorrhoids.In patients with thrombosed external hemorrhoids, early surgical excision should be attempted.
- Hemorrhoidectomy -Traditional hemorrhoidectomy remains very effective. When compared with office procedures, hemorrhoidectomy was more effective for grade III hemorrhoids, but more painful, and had a higher complication rate. Standard hemorrhoidectomy leaves open or closed wounds , and it may be performed with a variety of surgical devices, none of which displays a clear advantage over the other should typically be offered to patients whose symptoms result from external hemorrhoids or combined internal and external hemorrhoids with prolapse (grades III–IV) .Either open or closed hemorrhoidectomy can be performed with a variety of surgical devices.Studies suggest that the use of a bipolar energy device is faster and causes less postoperative pain as opposed to closed hemorrhoidectomy with comparable rates of postoperative complications.In addition ,Ultrasonic shears are associated with fewer postoperative complications compared to conventional hemorrhoidectomy
- Stapled Hemorrhoidopex-Stapled hemorrhoidopexy uses a circular stapler to resect a ring of tissue rostral to the anal cushions, and to remove redundancy in the remaining anal cushions. Being highly effective for prolapsing internal hemorrhoids and less painful than hemorrhoidectomy, it may not adequately address external hemorrhoids. Systematic reviews demonstrated slightly lower complication rates and higher long-term recurrence rates with stapled hemorrhoidopexy compared with standard hemorrhoidectomy.Stapled hemorrhoidopexy is an established alternative to hemorrhoidectomy in most cases.Stapled hemorrhoidopexy uses a circular stapling device to create a mucosa-to-mucosa anastomosis by excising the submucosa proximal to the dentate line, resulting in a cephalad relocation of the anal cushions and interruption of the feeding arteries.Stapled hemorrhoidopexy is effective for internal prolapsing disease, but not for external hemorrhoids.As compared to excisional hemorrhoidectomy, Stapled hemorrhoidopexy has been associated with several unique complications like, rectovaginal fistula, staple line bleeding, and stricture at the staple line
- Doppler-Guided Hemorrhoidectomy-Doppler-assisted hemorrhoidal artery ligation uses a Doppler-equipped anoscope to identify and ligate the arteries supplying internal hemorrhoids. A potential comparative benefit is that less tissue is excised, although this may not address the problem of redundancy, as well as other operations. Success rates are comparable to those reported for both hemorrhoidectomy and stapled hemorrhoidopexy, although there have yet to be comparative studies.
- Complications of Surgical Hemorrhoidectomy- The most common complications of Surgical Hemorrhoidectomy are hemorrhage and acute urinary retention
- Patients undergoing surgical hemorrhoidectomy should use a multimodality pain regimen to reduce narcotic usage and promote a faster recovery. Topical 2% Diltiazem ointment has been has been found to be effective in conventional hemorrhoidectomy whereas Topical nitroglycerin, surgical sphincterotomy, Liposomal bupivacaine have caused significant pain reduction in patients of excisional hemorrhoidectomy.
To Read the full guidelines log on to: doi: 10.1097/DCR.0000000000001030
complicationshemorrhoid-pattern bleedinghemorrhoidopexyhemorrhoidsLiposomal bupivacainesurgical sphincterotomy
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd