- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Antimicrobial prescribing in lower Urinary tract infection: NICE Guideline
NICE has released Guidelines on Urinary tract infection (lower) LRTI.
Following are the major recommendations:
Managing lower urinary tract infection
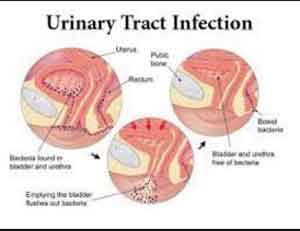
- Be aware that lower urinary tract infection (UTI) is an infection of the bladder usually caused by bacteria from the gastrointestinal tract entering the urethra and travelling up to the bladder.
- Give advice about managing symptoms with self-care to all people with lower UTI.
Treatment for women with lower UTI who are not pregnant
- Consider a back-up antibiotic prescription (to use if symptoms do not start to improve within 48 hours or worsen at any time) or an immediate antibiotic prescription for women with lower UTI who are not pregnant. Take account of: a) the severity of symptoms b) the risk of developing complications, which is higher in people with known or suspected structural or functional abnormality of the genitourinary tract or immunosuppression c) the evidence for backup antibiotic prescriptions, which was only in non-pregnant women with lower UTI where immediate antibiotic treatment was not considered necessary d) previous urine culture and susceptibility results e) previous antibiotic use, which may have led to resistant bacteria f) preferences of the woman for antibiotic use.
- If a urine sample has been sent for culture and susceptibility testing and an antibiotic prescription has been given: a) review the choice of antibiotic when microbiological results are available, b) change the antibiotic according to susceptibility results if bacteria are resistant and symptoms are not already improving, using a narrow-spectrum antibiotic wherever possible.
Treatment for pregnant women and men with lower UTI
- Offer an immediate antibiotic prescription to pregnant women and men with lower UTI. Take account of: a) previous urine culture and susceptibility results b) previous antibiotic use, which may have led to resistant bacteria.
- Obtain a midstream urine sample from pregnant women and men before antibiotics are taken, and send for culture and susceptibility testing.
- For pregnant women with lower UTI: a) review the choice of antibiotic when microbiological results are available, b) change the antibiotic according to susceptibility results if the bacteria are resistant, using a narrow-spectrum antibiotic wherever possible.
- For men with lower UTI: a) review the choice of antibiotic when microbiological results are available, b) change the antibiotic according to susceptibility results if the bacteria are resistant and symptoms are not already improving, using a narrow-spectrum antibiotic wherever possible.
Treatment for children and young people under 16 years with lower UTI
- Obtain a urine sample from children and young people with lower UTI before antibiotics are taken, and dipstick test or send for culture and susceptibility testing in line with the NICE guideline on urinary tract infection in under 16s.
- Assess and manage children under 5 with lower UTI who present with fever as outlined in the NICE guideline on fever in under 5s.
- Offer an immediate antibiotic prescription for children and young people under 16 years with lower UTI. Take account of:
- previous urine culture and susceptibility results
- previous antibiotic use, which may have led to resistant bacteria.
- If a urine sample has been sent for culture and sensitivity testing when an antibiotic prescription has been given: a) review the choice of antibiotic when microbiological results are available, b) change the antibiotic according to susceptibility results if the bacteria are resistant and symptoms are not already improving, using a narrow-spectrum antibiotic wherever possible.
Managing asymptomatic bacteriuria
- Be aware that asymptomatic bacteriuria: a) is significant levels of bacteria (greater than 105 colony forming units/ml) in the urine with no symptoms of UTI b) is not routinely screened for, or treated, in women who are not pregnant, men, young people and children c) is routinely screened for, and treated with antibiotics, in pregnant women because it is a risk factor for pyelonephritis and premature delivery.
- Offer an immediate antibiotic prescription to pregnant women with asymptomatic bacteriuria, taking account of: a) recent urine culture and susceptibility results b) previous antibiotic use, which may have led to resistant bacteria.
See the evidence and committee discussion on antibiotics.
Choice of antibiotic
Table 1 Antibiotics for non-pregnant women aged 16 years and over
| Antibiotic | Dosage and course length |
| First choice | |
| Nitrofurantoin – if eGFR ≥45 ml/minute4 | 100 mg modified-release twice a day for 3 days |
| Trimethoprim – if low risk of resistance5 | 200 mg twice a day for 3 days |
| Second-choice (no improvement in lower UTI symptoms on first-choice taken for at least 48 hours, or when first-choice not suitable) 3,6 | |
| Nitrofurantoin – if eGFR ≥45 ml/minute4 and not used as first-choice | 100 mg modified-release twice a day for 3 days |
| Pivmecillinam (a penicillin) | 400 mg initial dose, then 200 mg three times a day for a total of 3 days |
| Fosfomycin | 3 g single dose sachet |
| 1 See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment and breastfeeding. 2 Doses given are by mouth using immediate-release medicines, unless otherwise stated. 3 Check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly. 4 May be used with caution if eGFR 30–44 ml/minute to treat uncomplicated lower UTI caused by suspected or proven multidrug resistant bacteria and only if potential benefit outweighs risk (BNF, August 2018). 5 A lower risk of resistance may be more likely if not used in the past 3 months, previous urine culture suggests susceptibility (but this was not used), and in younger people in areas where local epidemiology data suggest resistance is low. A higher risk of resistance may be more likely with recent use and in older people in residential facilities. 6 If there are symptoms of pyelonephritis or the person has a complicated UTI (associated with a structural or functional abnormality, or underlying disease, which increases the risk of a more serious outcome or treatment failure), see the recommendations on choice of antibiotic in the NICE guideline on pyelonephritis (acute): antimicrobial prescribing. | |
| Abbreviations: eGFR, estimated glomerular filtration rate. | |
Table 2 Antibiotics for pregnant women aged 12 years and over
| Antibiotic | Dosage and course length |
| Treatment of lower UTI | |
| First choice | |
| Nitrofurantoin (avoid at term) – if eGFR ≥45 ml/minute4,5 | 100 mg modified-release twice a day for 7 days |
| Second-choice (no improvement in lower UTI symptoms on first-choice taken for at least 48 hours or when first-choice not suitable) 3,6 | |
| Amoxicillin (only if culture results available and susceptible) | 500 mg three times a day for 7 days |
| Cefalexin | 500 mg twice a day for 7 days |
| Alternative second-choices | Consult local microbiologist, choose antibiotics based on culture and susceptibility results |
| Treatment of asymptomatic bacteriuria | |
| Choose from nitrofurantoin4,5, amoxicillin or cefalexin based on recent culture and susceptibility results | |
| 1 See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment and renal impairment. 2 Doses given are by mouth using immediate-release medicines, unless otherwise stated. 3 Check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly. 4 Avoid at term in pregnancy; may produce neonatal haemolysis (BNF, August 2018). 5 May be used with caution if eGFR 30–44 ml/minute to treat uncomplicated lower UTI caused by suspected or proven multidrug resistant bacteria and only if potential benefit outweighs risk (BNF, August 2018). 6 If there are symptoms of pyelonephritis or the person has a complicated UTI (associated with a structural or functional abnormality, or underlying disease, which increases the risk of a more serious outcome or treatment failure), see the recommendations on choice of antibiotic in the NICE guideline on pyelonephritis (acute): antimicrobial prescribing. | |
| Abbreviations: eGFR, estimated glomerular filtration rate. | |
Table 3 Antibiotics for men aged 16 years and over
| Antibiotic | Dosage and course length |
| First choice | |
| Trimethoprim | 200 mg twice a day for 7 days |
| Nitrofurantoin – if eGFR ≥45 ml/minute4,5 | 100 mg modified-release twice a day for 7 days |
| Second-choice (no improvement in UTI symptoms on first-choice taken for at least 48 hours or when first-choice not suitable) 3 | |
| Consider alternative diagnoses and follow recommendations in the NICE guidelines on pyelonephritis (acute): antimicrobial prescribing or prostatitis (acute): antimicrobial prescribing, basing the antibiotic choice on recent culture and susceptibility results. | |
| 1 See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment and renal impairment. 2 Doses given are by mouth using immediate-release medicines unless otherwise stated. 3 Check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly. 4 Nitrofurantoin is not recommended for men with suspected prostate involvement because it is unlikely to reach therapeutic levels in the prostate. 5 May be used with caution if eGFR 30–44 ml/minute to treat uncomplicated lower UTI caused by suspected or proven multidrug resistant bacteria and only if potential benefit outweighs risk (BNF, August 2018). | |
| Abbreviations: eGFR, estimated glomerular filtration rate. | |
Table 4 Antibiotics for children and young people under 16 years
| Antibiotic 1 | Dosage and course length 2 |
| Children under 3 months | |
| Refer to paediatric specialist and treat with intravenous antibiotics in line with the NICE guideline on fever in under 5s. | |
| Children aged 3 months and over | |
| First choice | |
| Trimethoprim – if low risk of resistance | 3 to 5 months, 4 mg/kg (maximum 200 mg per dose) or 25 mg twice a day for 3 days 6 months to 5 years, 4 mg/kg (maximum 200 mg per dose) or 50 mg twice a day for 3 days 6 to 11 years, 4 mg/kg (maximum 200 mg per dose) or 100 mg twice a day for 3 days 12 to 15 years, 200 mg twice a day for 3 days |
| Nitrofurantoin – if eGFR ≥45 ml/minute | 3 months to 11 years, 750 micrograms/kg four times a day for 3 days 12 to 15 years, 50 mg four times a day or 100 mg modified-release twice a day for 3 days |
| Second-choice (no improvement in lower UTI symptoms on first-choice taken for at least 48 hours or when first-choice not suitable) | |
| Nitrofurantoin – if eGFR ≥45 ml/minute6and not used as first-choice | 3 months to 11 years, 750 micrograms/kg four times a day for 3 days 12 to 15 years, 50 mg four times a day or 100 mg modified-release twice a day for 3 days |
| Amoxicillin (only if culture results available and susceptible) | 1 to 11 months, 125 mg three times a day for 3 days 1 to 4 years, 250 mg three times a day for 3 days 5 to 15 years, 500 mg three times a day for 3 days |
| Cefalexin | 3 to 11 months, 12.5 mg/kg or 125 mg twice a day for 3 days 1 to 4 years, 12.5 mg/kg twice a day or 125 mg three times a day for 3 days 5 to 11 years, 12.5 mg/kg twice a day or 250 mg three times a day for 3 days 12 to 15 years, 500 mg twice a day for 3 days |
| 1 See BNF for children (BNFC) for appropriate use and dosing in specific populations, for example, hepatic and renal impairment. See table 2 if a young woman is pregnant. 2 The age bands apply to children of average size and, in practice, the prescriber will use the age bands in conjunction with other factors such as the severity of the condition being treated and the child's size in relation to the average size of children of the same age. Doses given are by mouth using immediate-release medicines, unless otherwise stated. 3 Check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly. Where a child or young person is receiving prophylactic antibiotics, treatment should be with a different antibiotic, not a higher dose of the same antibiotic. 4 If 2 or more antibiotics are appropriate, choose the antibiotic with the lowest acquisition cost. Some children may also be able to take a tablet or part-tablet, rather than a liquid formulation, if the dose is appropriate. 5 A lower risk of resistance may be more likely if not used in the past 3 months, previous urine culture suggests susceptibility (but this was not used), and in younger people in areas where local epidemiology data suggest resistance is low. A higher risk of resistance may be more likely with recent use and in older people in residential facilities. 6 May be used with caution if eGFR 30–44 ml/minute to treat uncomplicated lower UTI caused by suspected or proven multidrug resistant bacteria and only if potential benefit outweighs risk (BNFC, August 2018). 7 If there are symptoms of pyelonephritis or the person has a complicated UTI (associated with a structural or functional abnormality, or underlying disease, which increases the risk of a more serious outcome or treatment failure), see the recommendations on choice of antibiotic in the NICE guideline on pyelonephritis (acute): antimicrobial prescribing. | |
| Abbreviations: eGFR, estimated glomerular filtration rate. | |
To read the complete guidelines, click on the following link:
https://www.nice.org.uk/guidance/ng109
bladdercranberry productsDiarrhoeadipstick testgastrointestinal tractIllnessimmunosuppressionlower UTImicrobiological resultsnarrow-spectrumnauseaNICENICE 2018NICE guidelinepregnant womenpyelonephritisurethraurinary tract infectionurine alkalinisingurine cultureUTI
Source : With inputs from NICENext Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd