- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Antibiotic use linked to increased risk of colon cancer
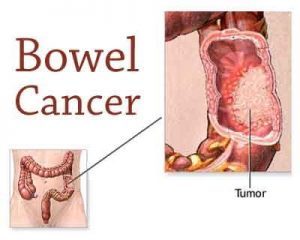
Antibiotic use is linked to a heightened risk of colon cancer, but a lower risk of rectal cancer, and depends, to some extent, on the type and class of drug prescribed, suggests research published online in the journal Gut.
The findings suggest a pattern of risk that may be linked to differences in gut microbiome (bacteria) activity along the length of the bowel and reiterate the importance of judicious prescribing, say the researchers.
In 2010, patients around the world took an estimated 70 billion doses of antibiotics--equivalent to 10 doses each. Antibiotics have a strong and long-lasting impact on the gut microbiome, altering the balance of helpful and harmful bacteria.
The researchers wanted to find out if this might affect bowel and rectal cancer risk, and how. They drew on data submitted to the nationally representative Clinical Practice Research Datalink (CPRD) between 1989 and 2012.
This contains the anonymised medical records of around 11.3 million people from 674 general practices--around 7% of the UK population.
The researchers collected prescribing information for 28,930 patients diagnosed with bowel (19,726 ) and rectal (9254) cancers during an average monitoring period of 8 years, and for 137,077 patients, matched for age and sex, who didn’t develop these cancers.
Antibiotics had been prescribed to 70% (20,278) of patients with bowel and rectal cancers and to 68.5% (93,862) of those without. Nearly six out of 10 study participants had been prescribed more than one class of antibiotic.
Those with bowel cancer were more likely to have been prescribed antibiotics: 71.5% vs 69%. Exposure levels were comparable among those who developed rectal cancer (67%).
The association between bowel cancer and antibiotic use was evident among patients who had taken these drugs more than 10 years before their cancer was diagnosed.
Patients who developed bowel cancer were more likely to have been prescribed antibiotics targeting anaerobes, which don’t need oxygen, as well as those targeting aerobes, which do--than patients without cancer.
But patients with rectal cancer were less likely to have been prescribed antibiotics targeting aerobic bacteria.
Cancer site was also associated with antibiotic use. Cancer of the proximal colon--the first and middle parts of the bowel--was associated with the use of antibiotics targeting anaerobes when compared to people without cancer.
But antibiotic use was not associated with cancer of the distal colon--the last part of the bowel.
After taking account of potentially influential factors, such as overweight, smoking, and moderate to heavy drinking, cumulative use of antibiotics for a relatively short period (16+ days) was associated with a heightened risk of bowel cancer, with the impact strongest for cancers of the proximal colon.
The reverse was true for rectal cancers, where antibiotic use exceeding 60 days was associated with a 15% lower risk compared with no use.
When the analysis was restricted to patients who had been prescribed only one class of antibiotic, as opposed to none, penicillins were consistently associated with a heightened risk of bowel cancer of the proximal colon. Ampicillin/amoxicillin was the penicillin most commonly prescribed to these patients.
By contrast, the lower risk of rectal cancer was associated with prescriptions of tetracyclines.
This is an observational study, and as such, can’t establish cause, and the researchers weren’t able to capture potentially influential lifestyle factors for all the participants, nor hospital treatment, which may have affected overall cancer risk.
Nevertheless, their findings suggest “substantial” variation in the size and pattern of antibiotic effects along the length of the bowel, they say, concluding: “Whether antibiotic exposure is causal or contributory to colon cancer risk, our results highlight the importance of judicious antibiotic use by clinicians.”
For more details click on the link: lifts: http://gut.bmj.com/lookup/doi/

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd