- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Ankylosing Spondylitis - Standard Treatment Guidelines
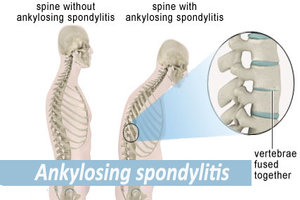
A form of spondyloarthritis, is a chronic, inflammatory arthritis and autoimmune disease. It mainly affects joints in the spine and the sacroiliac joint in the pelvis, and can cause eventual fusion of the spine.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Ankylosing Spondylitis. Following are the major recommendations :
Case definition
The typical patient is a young male, aged 20–40, however the condition also presents in females. The condition is known to be hereditary. Symptoms of the disease first appear, on average, at age 23 years. These first symptoms are typically chronic pain and stiffness in the middle part of the spine or sometimes the entire spine, often with pain referred to one or other buttock or the back of thigh from the sacroiliac joint.
Incidence of The Condition In Our Country
Three men are diagnosed with AS for every one woman; the overall prevalence is 0.25%. Many rheumatologists believe the number of women with AS is underdiagnosed, as most women tend to experience milder symptoms.
Differential Diagnosis
Differential diagnosis of Ankylosing Spondylitis include
1. Rheumatoid Arthritis
2. Other Spondylo arhtropathies
Prevention And Counseling
As no direct cause for the disease has been identified the preventive measures could not be established.
Patient needs to be counselled regarding the chronic nature of the disease and need for regular treatment, possible complications and possible treatment options and chances of improvement.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
SITUATION 1: At Secondary Hospital / Non Metro situation : Optimal standards of Treatment in situations where technology and resources are limited
Clinical Diagnosis :
chronic pain and stiffness in the middle part of the spine or sometimes the entire spine, often with pain referred to one or other buttock or the back of thigh from the sacroiliac joint. Post inactivity stiffness and morning stiffness. In 40% of cases, ankylosing spondylitis is associated with an inflammation of the eye (iritis and uveitis), causing redness, eye pain, vision loss, floaters and photophobia. This is thought to be due to the association these two conditions have with inheritance of HLA-B27. Other common symptoms are generalized fatigue and sometimes nausea.
Investigations:
1. X Ray
2. CT Scan
3. MRI
4. Complete Blood Picture
5. ESR
6. CRP
7. Liver function test
8. Renal function test
9. HLA B27
In a patient complaining of back pain of more than 12 weeks duration:
1. Morning stiffness of > 30 minutes
2. Improvement in back pain with exercise but not with rest.
3. Awakening because of back pain during the second half of the night only.
4. Alternating buttock pain.
5. Peripheral assymetrical large joint involvement.
6. Plain X Ray showing features of sacroilitis.
7. Absence of RA factor.
Any 2 out of first four criteria strongly indicate presence of Ankylosing Spondylitis even in the absence of xray and lab investigations.
Treatment:
not applicable.
Standard Operating procedure
In Patient
1. Surgery
- Joint Replacement for hip and knee.
Out Patient
- NSAIDS: First line therapy to relieve symptoms.
- DMARDs such as cyclosporin, methotrexate, sulfasalazine, and corticosteroids, used to reduce the immune system response through immunosuppression;
DMARDs are useful only for peripheral arthritis & not for axial skeleton involvement.
iii. Physical Therapy – Patients to be encouraged to undertake active and passive range of motion exercises for all joints to maintain and prevent the progression of loss of mobility. Deep breathing exercises (Pranayaam) should be promoted to improve chest function.
Day Care
1. Injectable medications
Referral criteria:
For further evaluation and management of cases not responding to conventional therapy.
SITUATION 2: At Super Specialty facility in Metro Location where higher end technology is available
Clinical Diagnosis :
chronic pain and stiffness in the middle part of the spine or sometimes the entire spine, often with pain referred to one or other buttock or the back of thigh from the sacroiliac joint. Post inactivity stiffness and morning stiffness. In 40% of cases, ankylosing spondylitis is associated with an inflammation of the eye (iritis and uveitis), causing redness, eye pain, vision loss, floaters and photophobia. This is thought to be due to the association these two conditions have with inheritance of HLA-B27. Other common symptoms are generalized fatigue and sometimes nausea.
Investigations:
1. X Ray
2. CT Scan
3. MRI
4. Complete Blood Picture
5. ESR
6. CRP
7. Liver function test
8. Renal function test
9. HLA B27
In a patient complaining of back pain of more than 12 weeks duration:
1. Morning stiffness of > 30 minutes
2. Improvement in back pain with exercise but not with rest.
3. Awakening because of back pain during the second half of the night only.
4. Alternating buttock pain.
5. Peripheral assymetrical large joint involvement.
6. Plain X Ray showing features of sacroilitis.
7. Absence of RA factor.
Any 2 out of first four criteria strongly indicate presence of Ankylosing Spondylitis even in the absence of xray and lab investigations.
Treatment:
not applicable.
Standard Operating procedure
In Patient
1. Surgery
- Joint Replacement for hip and knee.
- Corrective surgeries for spinal deformity
Out Patient
- As in situation 1. In addition to that
- 1. TNFα blockers (antagonists) such as etanercept, infliximab, golimumab and adalimumab (also known as biologics), are indicated for the treatment of and are effective immunosuppressants in AS as in other autoimmune diseases.
Day Care
1. Injectable medications
WHO DOES WHAT? And TIMELINES
Doctor
Early diagnosis and appropriate treatment. Counsel the patient for prevention of deformities and dietary advice.
Nurse
counseling the patient. Injectable treatment
Technician
Appropriate bracing manufacturing and application of braces Physiotherapy
RESOURCES REQUIRED FOR ONE PATIENT /PROCEDURE (PATIENT WEIGHT 60KGS)
(Units to be specified for human resources, investigations, drugs and consumables and equipment. Quantity to also be specified)
| Situation | Human Resources | Investigations | Drugs & Consumables | Equipment |
| 1. | Doctor Nurse Technician | 1. X Ray 2. CT Scan 3. MRI 4. Complete Blood Picture 5. ESR 6. CRP 7. Liver function test 8. Renal function test 9. HLA B27 | a. DMARDs b. NSAIDs c. Steroid d. Consumables for surgery | Lab equipment Imaging equipment Exercise equipments Equipments for Operating Room |
| 2. (In Addition to Situation 1) | Biologic Agents | Spinal Fixation implants |
Guidelines by The Ministry of Health and Family Welfare :
Dr. P.K. DAVE, Rockland Hospital, New Delhi
Dr. P.S. Maini, Fortis Jessa Ram Hospital, New Delhi
Reviewed By :
Dr. V.K. SHARMA
Professor
Central Instiute of Orthopaedics
Safdarjung Hospital
New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd