- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Angle Closure Disease - Standard Treatment Guidelines
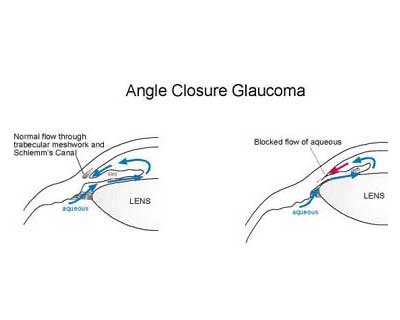
Angle closure implies either appositional or synechial closure of the anterior chamber angle. This iridotrabecular contact (ITC) may or may not be associated with raised intraocular pressure (IOP) or glaucomatous optic neuropathy. Various mechanisms are postulated in pathogenesis of primary angle closure (PAC), of which pupillary block constitutes a key element. This results in obstruction of aqueous flow from posterior chamber of eye to the anterior chamber, resulting in anterior bowing of iris and consequent crowding of the chamber angle. Prolonged apposition may lead to mechanical or functional obstruction to trabecular meshwork outflow and may result in formation of peripheral anterior synechiae (PAS), causing raised intraocular pressure and glaucomatous optic neuropathy. There are various other causes of ITC including position and thickness of ciliary body, iris thickness, lens position and thickness. Secondary angle closure can also occur in neovascularization, inflammation and gas or oil tamponade of posterior chamber besides other causes.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Angle Closure Disease. Following are the major recommendations :
Case definition:
Angle closure disease had been classified earlier on the basis of presence or absence of symptoms into three subtypes as acute, intermittent and chronic angle closure.Intermittent and chronic angle closure have since then been reclassified into PAC and PACG as described above.
In recent years, there has been an effort to standardize diagnostic definitions of angle closure glaucomas based on suggestions by International Society of Geographical and Epidemiological Ophthalmology (ISGEO). More emphasis is placed on structural (optic nerve head) and functional (visual field) changes to diagnose glaucoma. The amount of ITC (apposition between iris and posterior trabecular meshwork) required to define primary angle closure has been debated. By consensus, an eye with 180 degrees or more of ITC in dim illumination and non compressive gonioscopy is classified as one having primary angle closure disease. Based on associated findings this is further subclassified as:
Primary Angle Closure Suspect (PACS)
An angle where more than 180° of the posterior trabecular meshwork cannot be seen under dim illumination, which, in the presence of normal intraocular pressure and no disc/ field changes suggestive of glaucoma and no peripheral anterior synechiae is classified as primary angle closure suspect.
Primary Angle Closure (PAC)
An eye with PACS having peripheral anterior synechiae and/or raised intraocular pressure with no glaucomatous optic neuropathy is classified as primary angle closure.
Primary Angle Closure Glaucoma (PACG)
An eye with PACS having evidence of glaucomatous damage in the form of glaucomatous disc changes and/or visual field changes is classified as primary angle closure glaucoma. It is not mandatory to have raised intraocular pressure or peripheral anterior synechiae.
Secondary Angle Closure
Secondary angle closure occurs from known causes which may or may not be associated with pupillary block.
Etiology:
Secondary angle closure with pupillary block:
- Swollen lens induced (Phacomorphic)
- Anterior lens subluxation/ dislocation
- Trauma, laxity of zonules, Marfan’s syndrome
- Miotic induced secondary closure
- Miotics relax the ciliary muscle, causing forward movement of iris-lens diaphragm and may precipitate angle closure.
- Synechiae between iris and crystalline lens/ intraocular lens/cornea/ vitreous
- These cause a physical obstruction to flow of aqueous from the posterior to anterior chambers and may result in ‘iris bombe’.
- Aphakic pupillary block
Secondary angle closure with anterior pulling mechanism without pupillary block
- Neovascular glaucomas
- Iridocorneal endothelial syndromes
- Inflammation
- Post penetrating keratoplasty
- Epithelial downgrowth
- Aniridia
Secondary angle closure with posterior pushing mechanism without pupillary block
- Ciliary block glaucoma
- Iridociliary cysts
- Intravitreal silicon oil/ gas induced
- Ciliochoroidal effusions
- Suprachoroidal haemorrhage
- Scleral buckling
Incidence of The Condition In Our Country
Reported prevalence differences between studies occur due to differing methodology and classification of angle closure in these studies. The estimates of number of people with angle closure glaucoma in 2010 were 15.4 million for the world with India accounting for 3.7 million cases. Estimates of angle closure glaucoma in 2020 will rise to 21 million for the world and above 5 million for India.
The reported prevalence for PACG in Vellore eye study (VES) was 4.32%. In Andhra Pradesh Eye Disease Study (APEDS), the reported prevalence for PACG was noted to be 1.08% with another 2.21% having ‘occludable angles’. The criteria for occulability was different between the studies-the VES considered one half or more angle to be narrow to be considered occludable while APEDS had a criteria of three quarters or more. Moreover, VES incorporated PAC and PACG together into PACG. The actual prevalence of PACG would have been 0.5% alone. A similar prevalence of 0.5% for PACG was reported by Aravind Comprehensive Eye Survey (ACS).
The Chennai Glaucoma Study (CGS), using the current ISGEO criteria reported higher rates for PACS, PAC and PACG in the urban cohort as compared to rural one. The prevalence of PACG was noted to be 0.87% in rural and 0.88% in urban cohorts. Besides this, 6.3 % were classified as PACS and 0.7% as PAC in the rural cohort as compared to 7.2 and 2.8% in urban cohorts.
The prevalence of PACS has been noted to be higher than PAC and PACG in these, implying that all patients of PACS do not necessarily progress to PAC and PACG and the slow rate of conversion for the same.
Differential Diagnosis
- Secondary pupillary block due to uveitis with iris bombe
- Malignant glaucoma
- Lens induced angle closure-phacomorphic/ subluxation/ dislocation
- Neovascular glaucomas
Prevention And Counseling
The majority of patients are asymptomatic. Vision lost in glaucoma cannot be restored. The purpose of therapy is to preserve existing vision. Diagnosis of angle closure needs a detailed slit lamp examination, intraocular pressure assessment, indentation gonioscopy, optic nerve head assessment and investigations as required. Since cataract and glaucoma can coexist and the patient may attribute their vision loss to the former, it is essential to have a comprehensive eye examination above the age of 40 years at least annually or biannually. Being a progressive blinding disorder, if glaucoma is detected in a patient, the patient is counseled and explained the need for regular eye examinations throughout life. The need to screen close family members of the patient with angle closure disease is stressed as glaucomas at times may be heritable and may show familial predisposition.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis :
History:
Most primary angle closure glaucoma in Indian eyes is asymptomatic. A patient may present with intermittent attacks of redness or pain with halos and blurred vision in eyes or may present with acute onset of such symptoms. Previous or concomitant use of steroids in any form should be noted. Drugs likely to precipitate angle closure such as such as adrenergic and anticholinergic agents, tri and tetracyclic antidepressants, MAO inhibitors and sulfa based such as topiramate to be recorded along with any history of angle closure in family.
IOP:
Intraocular pressure is preferably assessed with Goldmann’s applanation tonometer.
Gonioscopy:
A carefully done goniosopy for diagnosis of angle closure is crucial and helps in follow up and management of these patients. Preferably, indentation gonioscopy is done in patients suspected for angle closure to differentiate appositional from synechial closure. It is first done in dim illumination with a short slit beam avoiding the pupil and then on indentation with a bright light. Excessive compression on the gonioscope and/ or excess light entering the pupil may artifactually open up the angle. Careful assessment of the angle structures with their exact anatomic documentation along with iris contour, iris processes, areas of peripheral anterior synechiae with pigmentation of the angle should ideally be done.
Optic nerve head and visual fields assessment:
Undilated disc assessment (if possible prior to laser peripheral iridotomy) with a +78/90 Dioptre lens under a slit lamp biomicrosope along with a dilated fundus examination with nerve fiber layer and optic nerve head assessment.
Investigations :
Automated perimetry (preferably Humphrey 24-2 SITA Standard/ Octopus G1 test) form the gold standard tests for the diagnosis and follow up of the glaucoma patient. In patients with advanced visual field losses 10-2 or macular threshold test on Humphrey may be required. Since visual fields may have a learning curve, it is preferable to have two visual fields with replicable defects to establish a reliable baseline. Serial stereoscopic disc photographs/disc drawings also form an important additional modality to follow up a patient.
Treatment:
Guidelines to therapy:
Treatment for angle closure revolves around intraocular pressure control, assessment and therapy directed to the control of the angle and angle closure, prevention and treatment for acute primary angle closure, preventing progression of glaucoma and thus aiming to preserve a patient’s vision and quality of life.
(1) Control of intraocular pressure:
Antiglaucoma medications are prescribed to control IOP for short term either before definitive therapy by laser or surgery and following the same for residual IOP elevation in the long term. All major classes of drugs can be used as for open angle glaucomas such as beta blockers, alpha agonists, carbonic anhydrase inhibitors, prostaglandin analogues, cholinergic agents and hyperosmotic agents can be used depending on their tolerability, side effects and contraindications. However Pilocarpine is usually contraindicated in lens induced and retro lenticular mechanisms as it may cause forward movement of iris lens diaphragm and shallowing of chamber angle. At low doses, Pilocarpine can be used for relieving residual appositional closure after laser iridotomy or iridoplasty in plateau iris and angle closure patients.
2) Angle control:
Laser peripheral iridotomy/ Surgical iridectomy
Preferably, a laser peripheral iridotomy (LPI) is done to alleviate pupillary block. It allows the aqueous to bypass the pupil, providing an alternative route for outflow from posterior to anterior chambers of the eye. Surgical iridectomy may rarely be needed in case of failures of laser iridotomy.
Laser peripheral iridotomy: Technique
The role and limitations and possible complications of laser iridotomy are explained to the patient. To reduce the risk of post laser IOP spike and inflammation, apraclonidine 1% or brimonidine 0.15/ 0.2% can be used either before or after the procedure.
Alternatively, oral/ topical carbonic anhydrase inhibitors or topical glycerine (in case of corneal epithelial edema secondary to raised IOP) can be used in selected patients. It is preferable to reduce IOP to a safe level prior to the procedure. To reduce the risk of bleeding, selected patients on oral anticoagulants for systemic diseases should be counseled and may be asked to stop their anticoagulants for a few days prior to the procedure. Usually iridotomy is recommended between 11-1 o’ clock beneath the eyelids avoiding the 12 o’ clock position. However, others prefer 3 and 9 o’ clock positions. PI is avoided at lid margins to reduce symptoms of glare formed by tear meniscus. Successful penetration is seen with a gush of pigments in anterior chamber with a visible deepening of anterior chamber. A minimum opening of 150-200 microns is aimed to ensure patency.
Parameters (Nd-YAG laser)
Energy: 2-5 mJ, 1-3 pulses/ burst
It is preferable to choose a thin area of iris or an iris crypt to reduce the amount of energy and associated complications with the procedure. Pre treatment with pilocarpine to stretch and thin the peripheral iris is helpful. Use of Abraham or Wise lenses with coupling agents is preferred to enhance magnification and focusing of the laser beam. Complications and follow up after LPI: Possible complications can include IOP spike, blurred vision, bleeding, damage to corneal epithelium or endothelium and rarely damage to lens capsule or the retina. Late complications include progression of cataract and iridotomy closure. Post laser IOP check is done within 1-6 hours and patient is advised tapering dose of topical steroids with antiglaucoma medications as needed. Reassessment of the angle after pilocarpine effect wears off with documentation of areas of synechial and appositional closure is done.
(3) Surgery: Surgery is usually considered in case of failure of medical/ laser management for IOP control or progression of glaucoma despite maximum medical management.
Trabeculectomy alone or combined with cataract surgery
Cataract surgery alone-helps to reduce crowding of the angle and relative pupillary block.
Treatment of primary angle closure disease:
PACS
As noted, not all patients of PACS progress to PAC or PACG. The treatment needs to be individualized in regards to laser iridotomy or a close follow up. An iridotomy may be considered to reduce the risk of angle closure in future or alternatively the patient may be monitored for IOP elevation and PAS over time. However an iridotomy can be considered in the following situations:
- Fellow eye of an eye with primary angle closure
- Confirmed family history of angle closure glaucoma
- Eyes requiring frequent dilation for retinal examination
- When follow up is impractical or a poorly compliant patient
- Symptomatic patient
- Difficulty in opening the angle with compression, with areas of patchy trabecular
meshwork pigmentation
In case iridotomy is deferred, patients are warned about symptoms of angle closure and are counseled for regular check ups. The possible risk of angle closure by medications such as decongestants and motion sickness is warned.
PAC and PACG
Laser peripheral iridotomy to relieve pupillary block is recommended as first line therapy. Appositional or synechial closure of the angle with concomitant damage to trabecular meshwork can cause rise in IOP. However, medical treatment should not be used as a substitution of laser in cases of PAC and PACG.
After component of pupillary block has been removed, further management on lines of open angle glaucomas is done to prevent pressure induced glaucomatous optic neuropathy and visual field progression by topical hypotensive agents and/or surgery.
Plateau Iris Configuration/ Syndrome
Elimination of element of pupillary block by LPI is recommended as first line of treatment. Iridoplasty helps opening up non synechial areas of the angle in selected patients. Chronic use of low dose miotic therapy may prevent further closure of the angle.
Acute Primary Angle Closure
Initial treatment is medical to lower IOP to a level when definitive therapy by LPI can be performed.
Medical therapy includes topical hypotensive agents and systemic agents to reduce IOP rapidly. However, topical mioics may not be effective at times in an ischemic pupillary sphincter. Indentation with a 4 mirror gonioscope or a cotton tipped applicator has been used to break the acute attack. Laser iridectomy of the affected eye is the definitive management. It is done along with prophylactic iridectomy of the fellow eye, if narrow. This is done as nearly 50% of fellow eyes have been reported to develop acute closure within 5 years of the fellow eye. Following LPI, reassessment of the angles by gonioscopy is done to determine extent of synechial closure. IOP is controlled by antiglaucoma medications and optic nerve head damage and visual field assessment is done to outline further management. In case of extensive synechial closure, incisional surgery for glaucoma can be considered for IOP control, although it carries a high risk of post operative complications such as shallow anterior chamber and malignant glaucoma.
Treatment of secondary angle closure glaucomas:
The treatment of secondary glaucomas is directed to the primary event causing angle closure which is based on the underlying mechanism of angle closure—pupillary block, or non pupil block (anterior pulling/ posterior pushing) mechanisms.
Thus, treatment of secondary glaucomas may require relief of pupil block (iris bombe/ lens induced) with YAG peripheral iridectomy and treatment of underlying in inflammatory disorder. Raised IOP is treated with topical/ oral antiglaucoma medications as needed.
Standard Operating procedure
a) In Patient
- Acute primary angle closure unresponsive to medical therapy/lasers
- Lens induced (Phacomorphic glaucoma)
- Symptomatic secondary angle closure requiring hyperosmotics for IOP control
b) Out Patient
- PACS, PAC, PACG, Secondary glaucomasAcute primary angle closure (following laser iridotomy and the patient is asymptomatic)c) Day Care
- Not applicable
Referral criteria:
Immediate referral on presentation if there is
Acute primary angle closure with uncontrolled IOP on maximum therapy and facilities for laser peripheral iridotomy are not available
Facilities for cataract surgery not available in lens induced glaucomas (phacomorphic) Children (acute intraocular pressure lowering measures initiated prior to referral; laser or surgical therapy to be done at higher centres)
Referral following initial treatment if,
- Secondary glaucomas without facilities to treat the underlying cause (for example laser iridotomy for pupil block/ surgery (ex. in microspherophakia or lensectomy for subluxated crystalline lens)
- Nanophthalmos requiring surgery
- Previous failed trabeculectomy uncontrolled on maximum antiglaucoma therapy
- Patients requiring tube implants
- Only seeing eye
- Post congenital cataract surgery with uncontrolled IOP on therapy
- Complications of filtration surgery requiring surgical intervention
- Failing bleb
Large choroidal haemorrhage/ effusions
Bleb leaks
Blebitis and endophthalmitis
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
The clinical diagnosis and management is done on the same general guidelines as given above.
Clinical Diagnosis:
A Perkins tonometer or Tonopen (especially in case of corneal scarring precluding the use of a Goldmann’s tonometer) may be used for IOP measurement
Investigations:
Ancillary investigations which may aid clinical diagnosis and management include
Imaging of anterior segment:
A carefully done gonioscopy remains the gold standard for diagnosis of angle closure. There are various imaging tools to help evaluate the anterior segment of the eye. Anterior segment optical coherence tomography and ultrasound biomicroscopy play a key role in selected patients with angle closure. Both allow qualitative and quantitative assessment of anterior segment of the eye, although AS-OCT is unable to assess structures posterior to the iris.
Biometry To assess the axial length, lens thickness and anterior chamber depth (Refer ‘Risk factors’ above)
Imaging of optic disc and nerve fibre layer
Use of HRT, GDx and OCT (Retinal nerve fiber layer assessment) (if available)
Treatment:
- Control of IOP as outlined above
- Angle control
Laser peripheral iridotomy
Both Argon and Nd-YAG lasers can be used either alone or sequentially to achieve an iridotomy. Use of Nd-YAG laser for iridotomy has been described above. In sequential use, photocoagulative effects of argon laser are combined with photodisruptive effects of Nd-YAG laser. This is especially useful in cases of thick irides and to reduce the risk of bleeding. Argon laser is used first to thin the iris and then the Nd-YAG laser is used for penetration.
| Parameters (Argon laser) | |
| Stretch Burns: | |
| Spot size: | 200-500 µm |
| Exposure time: | 0.2-0.5 sec |
| Power: | 200-600 mW |
| Penetration burns: | |
| Spot size: | 50 µm |
| Exposure time: | 0.02 sec |
| Power: | 800-1000 mW |
Argon laser peripheral iridoplasty.
(3) Surgery
Trabeculectomy alone or combined with cataract surgery
Cataract surgery alone-helps to reduce crowding of the angle and relative pupillary block.
Tube implant surgery
Management of complications of glaucoma surgery causing secondary closure of angle
Malignant glaucoma
- Aqueous suppressants/ cycloplegics (miotics are contraindicated)
- Nd-YAG hyaloidotomy along with posterior capsulotomy in pseudophakics
- -Pars plana vitrectomy
-Topical steroids/ cycloplegics with or without systemic steroids
- Choroidal drainage if conservative measures fail
Acute primary angle closure
Other modalities attempted include iridoplasty and paracentesis for temporary lowering of IOP. In case LPI is not possible, iridoplasty or surgical iridectomy can be attempted. Cataract surgery alone or combined with goniosynechiolysis have been reported with varying success rates. This approach may be attempted in eyes not amenable to laser iridotomy or surgical iridectomy, however the risks and benefits should be weighed beforehand.
Genetic counseling: This forms an important tool to educate and inform patients about higher risk of glaucoma in close relatives and children.
Standard Operating procedure
a)In Patient
- Patients requiring surgical intervention
- Acute primary angle closure with uncontrolled IOP on maximum therapy /laser peripheral iridotomy not complete (symptomatic patient)
- Lens induced glaucomas (phacomorphic)
- Blebitis and Endophthalmitis
- Malignant glaucoma refractory to medical management
b)Out Patient
- PACS, PAC, PACG, Secondary glaucomas
- b)Day Care
- Not applicable
Referral criteria:
- Not applicable
WHO DOES WHAT? And TIMELINES
Doctor
- Clinical history and examination
- Visual acuity
- Intraocular pressure measurement
- Gonioscopy
- Undilated/ dilated fundus examination
- ASOCT/ UBM
- YAG peripheral iridotomy/ Iridoplasty
- Surgery if indicated
Nurse/Technician
- Preparing the patient for laser treatment
- Ancillary tests-Pachymetry, Visual fields, Disc photography
- Compliance to therapy for inpatients
FURTHER READING / REFERENCES: Please refer at the end of the chapter
Resources Required
| Situation | HUMAN RESOURCES | INVESTIGATION S | DRUGS & CONSUMABLES | EQUIPMENT |
| 1) Secondary level | 1)Ophthalmologist -1 2)Optometrist/ Technician -1 3)OP Nurse -1 | 1)Visual fields 2)Pachymetry 3)Disc photographs (desirable) | 1)Antiglaucoma medications 2)Topical steroids 3)Irrigating Solutions 4)Viscoelastic agents 5)Mydriatics & Cycloplegics 6)Antibiotic eye drops 7)Intraocular lenses 8) Needle and syringes 9) Suture materials | 1)Slit lamp biomicroscope-1 2)Goldmann applanation tonometer -1 3)Indentation gonioscope -1 (preferable Sussman/ Posner/ Zeiss) 4)90D/ 78 D lens-1 5)Indirect ophthalmoscope-1 6)Operating Microscope 7)Microsurgical Instruments 8)Pachymeter 9)Nd-YAG laser 10)Lenses for PI-1 (Abraham/ Wise) 11)Automated perimeter-1 (preferably 12)Humphrey/ Octopus) |
| 2) Tertiary level | 1)Glaucoma specialist-1 2)Optometrist/ Technician -1 3)OP Nurse -1 4)Scrub nurse -1 5)OT nurse - 1 6)Ward nurse - 1 7) Counsellor - 1 | 1)Visual fields 2)Pachymetry 3)Biometry 4)ASOCT (desirable) 5)UBM 6)Ultrasound 6)Disc photographs | 1)Antiglaucoma medications 2)Topical/Systemi c steroids 3)Irrigating Solutions 4)Viscoelastic agents 5)Mydriatics & Cycloplegics 6) Antibiotic eye drops 7)Antimetabolites 8)Ologen 9)Glaucoma Drainage Devices 10)Intraocular lenses 11) Needles & Syringes 12) Suture materials | 1)Slit lamp biomicroscope-1 2)Goldmann applanation tonometer-1 3)Indentation gonioscope-1 (preferable Sussman/ Posner/ Zeiss) 4)90D/ 78 D lens-1 5)Indirect ophthalmoscope-1 6) Pachymeter 7)Ultrasound-1 8)Disc photography-1 9) A Scan-1 10)Diode laser with laser delivery system / Cryo-1 (recurring supplies required for G probe for Diode) 11)Nd-YAG laser-1 12)Automated perimeter-1 (preferably Humphrey/ Octopus) 13)ASOCT-1 14)UBM-1 15)Lenses for PI / Iridoplasty -1 16)Operating Microscope 17)Microsurgical Instruments |
Guidelines by The Ministry of Health and Family Welfare :
Dr. Venkatesh Prajna Chief- Dept of Medical Education, Aravind Eye Hospitals, Madurai

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd