- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Angioplasty in diabetes, special considerations
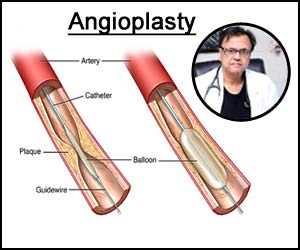
Several meta-analyses are giving compelling evidence that coronary artery bypass surgery is a preferred way of revascularization in diabetes patients. Hyperglycemia, high blood sugar, insulin resistance, and altered free fatty acid metabolism which is found in diabetes changes the inflammatory pathway causing severe endothelial dysfunction and increased coronary artery plaque burden and plaque instability. The re-stenosis and incidence of stent thrombosis are very high in patients with diabetes Mellitus leading to more Major Adverse Cardiovascular Events (MACE) after percutaneous angioplasty.
It has been noted that a major issue in survival and MACE in diabetes after PCI (Percutaneous Coronary Intervention) have been a complete or incomplete revascularization. PCI has been associated with more incidence of repeat revascularization since, more often it causes incomplete revascularization. and also since the revasculaeizatrion is lesion specific it doesn’t give immunity from future lesion formation and development of symptoms.
CABG is associated with more complete form of revascularization due to utilization of Left Internal Mammary Artery (LIMA) to left anterior descending artery (LAD). The bypass graft not only bypasses the present lesions but also bypasses any future lesions in the same artery and thus is assocated with lesser incidence of repeat revas.
While LEMA graft are definitely superior to the LED revascularization the saphenous vein grafts are not superior to the stents in the Left circumflex artery (LCS) and Right coronary artery.
Thus, many investigators are now recommending a hybrid approach where the LIMA is utilized to revascularize LAD and coronary artery stents substitute other grafts in LCX and RCA giving the best of both the strategies.
If at all, large surgical risk and patient preferences are forcing PCI as a primary strategy then the operator must be conscious of the following issues and the special considerations are required to perform the procedure of angioplasty.
It is now known that diabetes causes severe myocardial dysfunction and infect causes a sort of cardiomyopathy with more Left Ventricle (LV) dysfunction. There is 30% increase in the congestive heart failure in diabetic patients even in the absence of CAD, Hypertension and other risk factors. While doing PCI in diabetic patients myocardial dysfunction should be specifically looked for and the left-sided failure should be managed adequately with hemodynamic stabilization before taken on to any intervention.
Diabetes is an independent risk factor for Contrast-Induced Nephropathy (CIN). The risk of CIN should be calculated separately with its associations with other clinical issues like Hypotension, CHF age more than 75, Anemia, along any with existing CKD (Chronic kidney disease) in all patients of diabetes. The ultra-low contrast strategy should be used in all diabetic patients. The adequate hydration, use of low-osmolar contrast and 1ml/GFR strategy is found to be useful in preventing CIN
It should be known that vascular access is often more difficult because in diabetic patients there is 2.5 times more incidence of Peripheral Artery Disease. There is an increased incidence of potential infection with indwelling sheaths in diabetic patients. It is known to all that healing is severely compromised in diabetics.
Various meta-analysis has shown that there are higher rates of post-angioplasty deaths due to MI and repeat Target Vessel Revascularization (TVR). There is an increased atherosclerotic burdens in diabetic patients with diffused disease and the lesion may be more negatively remodeled. This gives a potential risk of perforation if aggressive stent sizing approach is applied.
There is a higher risk of stent thrombosis because of strong prothrombotic milieu and requires aggressive and monitored antiplatelet therapy. It is seen that clopidogrel resistance is more in diabetic patients and Prasugrel was found to be much better then clopidogrel if not contraindicated by weight and age.
It should be noted that the hyperglycemia at the time of PCI or after the PCI carries an enormous increase in MACE and control of glucose levels in peri-intervention periods as well as the optimum control of diabetes after the intervention with adequate control of HBA1C, hypertension, high lipids is mandatory. All the treatment of diabetes after intervention should be weight neutral.
Not all the diabetics behave the same after angioplasty. The patients taking insulin have got worst outcome because insulin plaque in stabilization.
SYNTAX II strategy of doing PCI improves outcomes in diabetic patients which includes
- heart team decision utilizing syntax core II to decide the modality of revascularization,
- Physiology guided revascularization,
- Implantation of thin strutsbioresorbable polymer drug-eluting stent,
- Intravascular ultrasound-guided stent implantation,
- Contemporary chronic total occlusion (CTO) revascularization technique ,
- Guideline directed medical therapy for control of diabetes hypertension, Hyperlipidemia,
- Natural weight treatment
- physical exercise
All this should be used and found superior than the classical PCI approach in diabetic patients.
In conclusion in a diabetic patient, a PCI can be performed and all extra incidence of MACE can be controlled by certain special consideration, use of special devices and adoption special strategies.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd