- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Anesthetic management of a patient with Steinert disease- case report
Dr Décia Gonçalves at Centro Hospitalar de Leiria, Rua das Olhalvas, Portugal and colleagues have reported Anesthetic management of a patient with Steinert disease in Journal of Clinical Anesthesia.
In addition to the challenges related to multiple organ dysfunction, these patients also present a variable clinical response to the commonly used anesthetics, analgesics, and neuromuscular relaxants.
The authors have presented a 46-year-old male patient diagnosed with SD, proposed for elective laparoscopic cholecystectomy for cholelithiasis.
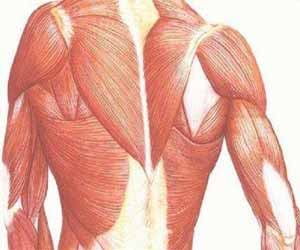
The patient had temporal muscle atrophy, bilateral facial paresis, mild dysarthria, episodes of myotonia of the hands and gait with support. Axial musculature, upper and lower limbs with atrophy and muscular strength grade 4, according to the Muscular Impairment Rating Scale. All the preoperative exams were normal. The proposed procedure was explained and the patient consented.
It was decided to perform total intravenous anesthesia (TIVA). Administered ranitidine 150 mg and metoclopramide 10 mg for prophylaxis of pulmonary aspiration of gastric contents, 60 min prior to induction. The patient was monitored according to standards of the ASA and with Bispectral Index (BIS®). Heating maneuvers were started, aiming a temperature above 36 °C (oesophageal temperature monitoring). After prophylactic antibiotic and pre-oxygenation, perfusion of propofol (target-controlled infusion [TCI], Schneider model) at 4 μg/ml was initiated and, 30 s later, remifentanil (TCI, Minto model) at 4 ng/ml. After reaching a BIS® value below 50, orotracheal intubation was performed, without neuromuscular relaxation and without incidents. Anesthesia was maintained with propofol TCI between 3 and 6 μg/ml and remifentanil between 3 and 8 ng/ml, according to BIS® value and vital signs. Administered ketamine 0.5 mg/kg.
Applied standard four-ports laparoscopic technique, with pneumoperitoneum pressure of 12 mm Hg. The surgery ran for 55 min, without technical difficulty and surgical incisions were infiltrated with ropivacaine 0.5%. Administered droperidol 1,25 mg and ondansetron 4 mg, as prophylaxis of nausea and vomiting, paracetamol 1 g and tramadol 2 mg/kg intravenously. Hemodynamic stability was maintained, without episodes of myotonia or unpredictable pharmacological response.
The emergency of the anesthesia was smooth, with extubation of the patient after recovery of the ventilatory drive, protective reflexes of the airway and level of consciousness. The patient remained in the post-anesthetic care unit for 4 h, requiring administration of metamizole 2 g intravenously to control postoperative pain. Presented conditions for discharge the next day, with cardiorespiratory stability and pain control.
In this case, we have tried to minimize the risk of cardiorespiratory complications, myotonia and side effects of the drugs. Contrary to what was previously advocated, there appears to be no increased risk of malignant hyperthermia in these patients, when compared to the rest of the population. However, considering the possibility of unpredictable response to neuromuscular blocking drugs and their reversers, we chose to perform a TIVA without neuromuscular block. Although the potential of remifentanil secondary hyperalgesia, this was not observed in this case. The administration of propofol did not induce episodes of myotonia and presented an expected pharmacodynamic profile, corroborating the reported safe cases. The established multimodal analgesia contributed to the comfort of the patient, avoiding the use of opioid drugs in the postoperative period and the possibility of respiratory depression.
Considering the high complexity of SD, the success of its approach depends on multidisciplinary planning and involvement from the preoperative period to postoperative monitoring. The case reported suggests that TIVA with propofol and remifentanil, without neuromuscular block, is safe and provides satisfactory operative conditions for a patient with SD undergoing laparoscopic cholecystectomy. The patient has provided written consent to present his case.
Declaration of Competing Interest
The authors did not receive financial aid for this work and declare no conflicts of interest.
For more details click on the link: https://doi.org/10.1016/j.jclinane.2019.06.016

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd