- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Amoxicillin–clavulanate remains first-line antibiotic for pediatric bronchiectasis: BEST-1 Study
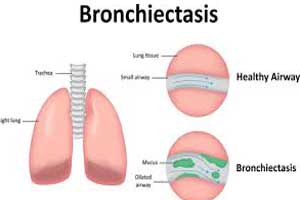
Amoxicillin–clavulanate treatment should remain the first-line antibiotic for the resolution of nonsevere acute exacerbations in children with non-cystic fibrosis (CF) bronchiectasis, emphasizes BEST-1 study published in The Lancet Respiratory Medicine journal.
Guidelines on bronchiectasis recommend antibiotics for the treatment of acute respiratory exacerbations, but there is a lack of randomized controlled trials (RCTs) in children.
Vikas Goyal, Department of Respiratory and Sleep Medicine, Queensland Children's Hospital, Brisbane, Australia, and colleagues in this multicentre, three-arm, parallel, double-dummy, double-blind set out to determine whether oral amoxicillin-clavulanate and azithromycin would each be superior to placebo in achieving symptom resolution of non-severe exacerbations in children by day 14 of treatment.
For the purpose, the researchers enrolled 252 children after screening 604 children between April 17, 2012, and March 1, 2017. The children had CT-confirmed bronchiectasis unrelated to cystic fibrosis who were under the care of a respiratory physician and who had at least two respiratory exacerbations in the 18 months before study entry. They were then allocated at exacerbation onset to receive oral suspensions of amoxicillin-clavulanate (45 mg/kg per day) plus placebo azithromycin, azithromycin (5 mg/kg per day) plus placebo amoxicillin-clavulanate, or both placebos for 14 days.
197 children were allocated at the start of an exacerbation (63 to the amoxicillin–clavulanate group, 67 to the azithromycin group, and 67 to the placebo group).
The primary outcome was the proportion of children with exacerbation resolution by day 14 in the intention-to-treat population
Key findings include:
- Respiratory viruses were identified in 82 (53%) of 154 children with available nasal swabs on day 1 of treatment.
- Primary outcome data were available for 196 (99%) children (one child with missing data [placebo group] was recorded as non-resolved according to criteria defined a priori).
- By day 14, exacerbations had resolved in 41 (65%) children in the amoxicillin-clavulanate group, 41 (61%) in the azithromycin group, and 29 (43%) in the placebo group.
- Compared with placebo, the relative risk for resolution by day 14 was 1·50 in the amoxicillin-clavulanate group and 1·41 in the azithromycin group.
- Adverse events were recorded in 19 (30%) children in the amoxicillin-clavulanate group, 20 (30%) in the azithromycin group, and 14 (21%) in the placebo group, but no events were severe or life-threatening.
“These results confirm the current recommendations for the use of amoxicillin-clavulanate to treat nonsevere exacerbations in children with bronchiectasis,” said the researchers. “Amoxicillin–clavulanate should remain the first-line antibiotic treatment for nonsevere exacerbations of bronchiectasis in children.”
“Taken together with our previously published non-inferiority RCT comparing amoxicillin-clavulanate and azithromycin, amoxicillin-clavulanate should remain the first-line antibiotic treatment for nonsevere exacerbations of bronchiectasis in children,” the researchers concluded.
“Azithromycin could be reserved for use in selected settings, such as in patients with genuine penicillin hypersensitivity or in situations in which less frequent, supervised dosing might overcome difficulties with adherence,” they advised.
To read the complete study log on to https://doi.org/10.1016/S2213-2600(19)30254-1

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd