- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
AIIMS Guidance on Empyema Thoracis
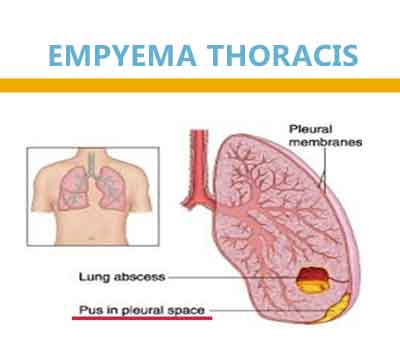
Empyema Thoracis is a collection of pus in the pleural space. It is divided into three stages: exudative, fibrinopurulent and organizing.
When to suspect
Failure of a community or healthcare-associated pneumonia to respond to antibiotic therapy (20- 40% cases of pneumonia have a parapneumonic effusion, and 5-10% of these parapneumonic effusions may progress to empyema).
How to confirm
Imaging:
1) CXR (PA view): at least 175ml is required
2) USG: Complex septated, complex non-septated and echogenic pleural effusions
3) CT Scan: Parietal pleural thickening (86%), pleural enhancement (96%) and Split Pleura sign (68%). High attenuation of the extrapleural adipose tissue in the chest wall.
Pleural Fluid Analysis: Pus or positive gram stain/culture is diagnostic of empyema.
Other diagnostic clues: pH<7.2, raised LDH, low glucose and high protein levels.
Note: Tuberculosis needs to be ruled out in all cases (ZN stain, gene Xpert, Liquid cultures, ADA levels)
[Specimens for culture should be collected during aspiration or drainage into aerobic and anaerobic blood culture bottles/ RCM bottles (available at anaerobic lab, room no. 2079) and sterile containers and not from previously inserted tubes or drains]
Aetiology:
Most common causes of non-tubercular empyema: Streptococcus pneumoniae followed by Staphylococcus aureus, Klebsiella pneumoniae, Haemophilus influenzae type b and Enterococcus sp.
Anaerobic causes are rare: Peptostreptococci, Bacteroides sp.
Post-procedure/ hospital-acquired: MRSA and Gram-negative bacilli
Treatment
Principles of management:
All patients with empyema need to be managed in a hospital.
An image-guided pleural drain must be put for all patients and large bore catheters should be preferred.
Tube thoracostomy should be combined with close CT or USG follow up to confirm the adequacy of drainage. Persistence of any undrained fluid should prompt additional drains or more aggressive management.
Ideal frequency and volume of flushing are not well established. Flushing with 20cc of sterile saline every 6 hours has shown to reduce occlusion rate.
Intrapleural fibrinolytic should NOT be used ROUTINELY for complicated pleural effusions and early empyema.
Management of Chronic empyema which has organised and is compromising lung expansion is mainly surgical.
a) For community-acquired empyema: (No risk for MDR organism)
*Cover anaerobes empirically even if cultures are negative
Preferred: [Amoxicillin-Clavulanate 1.2g IV TDS OR Ceftriaxone 1g IV 12th hourly] plus [clindamycin 600mg IV TDS OR metronidazole 500mg IV QID]
Alternative: Piperacillin/Tazobactam 4.5g IVQID
b) Community-acquired with risk factors for MDR- Previous antibiotic therapy, recent hospitalization, immunosuppression, pulmonary comorbidity, probable aspiration, and multiple medical comorbidities (eg, diabetes mellitus, alcoholism)
Preferred: Cefoperazone/Sulbactam 3g IV BD to TDS OR Piperacillin/Tazobactam 4.5g IV QID
Alternative: Imipenem-cilastatin500 mg QID OR Cefepime 2g IV TDS plus clindamycin 600mg IV TDS OR metronidazole 500mg IV QID
Post procedure (Cover MRSA):
Preferred: Cefoperazone/Sulbactam 3g IV BD to TDS or Piperacillin/Tazobactam 4.5g IV QID PLUS Teicoplanin 400mg IV 12th hourly for 3 doses followed by 24th hourly or Vancomycin 15 to 20mg/kg/dose 8th to 12th hourly2
Alternative: Imipenem-cilastatin500 mg QID PLUS Teicoplanin 400mg IV 12th hourly for 3 doses followed by OD or Vancomycin 15 to 20mg/kg/day 12th hourly
Special remarks:
Presence of air bubbles within the pleural effusion in the absence of preceding pleural intervention: specific for a pleural space infection- may suggest resistance to chest tube drainage alone.
A pleural pH < 7.2, LDH > 1000 IU/L, glucose < 40 mg/dL or a loculated pleural effusion predicts a complicated clinical course.
Avoid aminoglycosides (inactivated in empyema fluid)
Change antibiotics when culture and sensitivity reports are available
Intravenous to oral antibiotic switch:
If the patient has responded to therapy and there has been source control, then a transition to oral therapy can be made.
Switch to oral therapy can be made only when the organism is susceptible to oral antibiotics.
Switch to oral antibiotics in culture-negative cases should not be done.
References
F.J.H. Brims, S.M. Lansley, G.W. Waterer, Y.C.G. Lee. Empyema thoracis: new insights into an old disease.European Respiratory Review 2010; 19: 220-228.
K. Robert Shen, Alejandro Bribriesco, Traves Crabtree, Chad Denlinger, Joshua Eby, Patrick Eiken, David R. Jones, ShafKeshavjee, Fabien Maldonado, Subroto Paul, and Benjamin Kozower. The American Association for Thoracic Surgery consensus guidelines for the management of empyema. J Thorac Cardiovasc Surg 2017.
RashnaDass, Nayan Mani Deka, Himesh Barman et al. Empyema Thoracis: Analysis of 150 Cases from a Tertiary Care Centre in North East India, Indian J Pediatr 2011; 78(11):1371–1377.
P. Malhotra, A.N. Aggarwal, R. Agarwal, et al. Clinical characteristics and outcomes of empyema thoracis in 117 patients: A comparative analysis of tuberculous vs. non-tuberculous aetiologies, Respiratory Medicine 2007;101, 423–430.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd