- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
AIDAA guidelines for tracheal Intubation in ICU
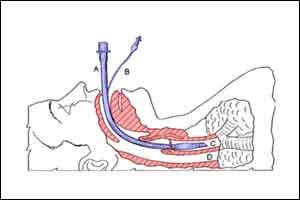
Tracheal Intubation in the ICU is a potentially hazardous procedure, most commonly due to failing oxygenation and unstable haemodynamics during emergency intubations. The AIDAA stepwise approach emphasises the importance of adequate supervision, good pre-oxygenation with non-invasive ventilation or HFNC oxygen at 60 L/min, maintenance of haemodynamic stability, use of IPPV with PEEP before intubation and insufflation of oxygen at 15 L/min or HNFC oxygen throughout the period of apnoea.
Step 1: Pre‑oxygenation and induction of anaesthesia
During intubation, the presence of minimum two persons is required, of which one should be experienced in airway management. Pre-oxygenation should be done, in the head-elevated position, if possible, using non-invasive ventilation with a pressure support ventilation level between 5 and 15 cm H2O to obtain an expiratory tidal volume between 6 and 8 mL/ kg and PEEP of 5 cm H2O (nasal cannula with an oxygen flow of 15 L/min may be used in addition when there is a mask leak) or HFNC with 70 L/min of oxygen flow should be used. Pre-intubation fluid loading with 500 mL of saline should be given in the absence of cardiogenic pulmonary oedema. The patient should be anaesthetised using ketamine or etomidate and neuromuscular blockade provided with succinylcholine or rocuronium. Intermittent positive pressure ventilation (IPPV) may be performed using bag-valve mask with reservoir bag using external PEEP valve set to 5–10 cmH2 O PEEP if available or IPPV using the ventilator maintaining a cricoid pressure throughout. Cricoid pressure should be given but may be partially or completely released if ventilation is inadequate.
Step 2: Laryngoscopy and tracheal intubation
If mask ventilation is successful, proceed with TI using direct or video laryngoscopy. Nasal oxygen using oxygen flow of 15 L/min or HFNC oxygen should be continued. Do not exceed more than two attempts at intubation and repeat an attempt only if the oxygen saturation (SpO2 ) is ≥95%. Mask ventilation should be performed between attempts. Optimise position, use external laryngeal manipulations, partially or completely release the cricoid pressure to optimise the laryngoscopic view if required and use a bougie or stylet if required. Between attempts at intubation, consider changing the device or technique, rather than repeating the same technique. Maintain depth of anaesthesia throughout the intubation attempts. If mask ventilation is
not possible, a single attempt at intubation could be made, provided the SpO2 is ≥95%. After intubation, confirm proper endotracheal tube (ET) tube position using capnography along with clinical methods.
Step 3: Insert supraglottic airway device to maintain oxygenation
If two attempts at intubation fail, or after a single attempt at intubation following unsuccessful mask ventilation fails, insert a SAD (preferably a second generation device) and ventilate to maintain oxygenation. Not more than two attempts should be made to insert an SAD and only if the SpO2 is ≥95%. Nasal oxygen using oxygen flow of 15 L/min or HFNC oxygen should be continued during SAD insertion. Perform mask ventilation between the
attempts. Consider using a different type or size of SAD during the second attempt. Maintain depth of anaesthesia throughout the insertion attempts. Once SAD insertion is successful and oxygenation is maintained, consider performing a percutaneous or surgical tracheostomy for further airway management. Intubation through the SAD may be considered, but only under vision using a flexible fibre-optic bronchoscope. Intubation should not be attempted blindly through the SAD if a bronchoscope and the expertise to use it are unavailable.
Step 4: Rescue face mask ventilation
If ventilation through the SAD fails, continue nasal oxygenation using oxygen flow of 15 L/min or HFNC oxygen. Ensure
complete neuromuscular blockade, repeat a muscle relaxant if required. Give one final attempt at face mask ventilation using optimal technique and adjuncts. If rescue face mask ventilation is successful, proceed with a percutaneous or surgical tracheostomy. However, if rescue face mask ventilation is unsuccessful, there is ‘complete ventilation failure’. Continue nasal oxygenation using oxygen flow at 15 L/min or HFNC oxygen and call for additional help. Immediately, start performing emergency cricothyroidotomy before the patient desaturates further.
Step 5: Emergency cricothyroidotomy
Perform emergency cricothyroidotomy using the needle or surgical cricothyroidotomy, based on familiarity and availability of equipment. If needle cricothyroidotomy is performed, maintain oxygenation using pressure-regulated jet ventilation, until a tracheostomy is performed. If a wide bore cannula cricothyroidotomy set has been used or an ET tube has been passed through the front of the neck, continue ventilation manually or using a ventilator circuit.
For more details click on the link: http://www.ijaweb.org/text.asp?2016/60/12/922/195485

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd