- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
ADAPT-DES Trial: 1 in 8 patients with PCI-DES have increased mortality
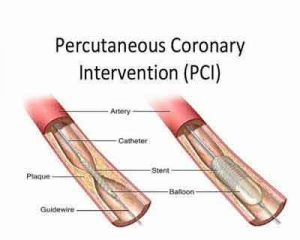
1 in 8 patients undergoing successful PCI with DES implantation experience clinically relevant bleeding, MI, or stent thrombosis during the ensuing 2 years
Ischemic and hemorrhagic events after percutaneous coronary intervention (PCI) with drug-eluting stents (DES) are strongly associated with subsequent death. Large number of patients despite of getting recommended drugs or with break in the death schedule gets ischemic / complications
In an analysis, Brener et al sought to understand the impact of the timing of these events using data from the multicenter, prospective ADAPT-DES (Assessment of Dual Antiplatelet Therapy With Drug Eluting Stents) study.
In ADAPT-DES, 8,582 patients at 11 clinical sites who had successful PCI with DES underwent assessment of platelet function and were followed for 2 years. Dual antiplatelet therapy (DAPT) was recommended for at least one year and aspirin was continued indefinitely. Adverse events were categorized as early (≤30 days), late (31 to 365 days), or very late (>365 days), and their relationship with subsequent mortality within 30 days were modeled using Kaplan-Meier methods.
A total of 1,060 patients (12.4%) had ischemic or hemorrhagic events: 8.1% of patient had clinically-relevant bleeding, 3.4% had a myocardial infarction (MI) not related to stent thrombosis, and 0.9% had stent thrombosis.
The highest risk of death was associated with early stent thrombosis, with an absolute rate of death of 38.5% at 30 days after the event, or about double that seen for late or very late stent thrombosis. For MI, the very late events were associated with the highest death rate at 30 days: a 10-fold increase compared with early MI and an absolute rate of 7.5%. Late clinically relevant bleeding was associated with a mortality rate similar to MI (7.3%).
On multivariate modeling, stent thrombosis, clinically relevant bleeding, and MI without stent thrombosis were all significant predictors of 2-year mortality.
The investigators concluded that about 1 in 8 patients undergoing successful PCI with DES implantation experience clinically relevant bleeding, MI, or stent thrombosis during the ensuing 2 years. All of these events are associated with increased mortality risk, in particular early stent thrombosis, which was associated with a 38.5% mortality rate within 30 days of the event.
In an editorial that accompanied this report, Dr. D Cutlip cautioned against seeing the lower mortality rate after very late stent thrombosis after discontinuation of DAPT as a cause for “complacency” since, while its occurrence was relatively rare, the 30-day mortality after very late stent thrombosis was still 20%, or nearly 3-fold higher than spontaneous MI or clinically-relevant bleeding at any time point. He added that, beyond 30 days, MI and clinically relevant bleeding are “equally important complications,” and to the extent that patients can be identified as being at higher risk for one or the other, “the goal should be to move away from dogmatic DAPT strategies toward adapting DAPT for personalized care and improved overall outcomes.”
References
- 1 Brener SJ, Kirtane AJ, Stuckey TD, et al.The impact of timing of ischemic and hemorrhagic events on mortality after percutaneous coronary intervention. The ADAPT-DES study. JACC CardiovascInterv. 2016; 9: 1450-7.
- 2 Cutlip DE. Adapting DAPT to improve outcomes after coronary stenting. JACC CardiovascInterv. 2016; 9: 1458-60.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd