- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Acute Pulmonary Embolism - Standard Treatment Guidelines
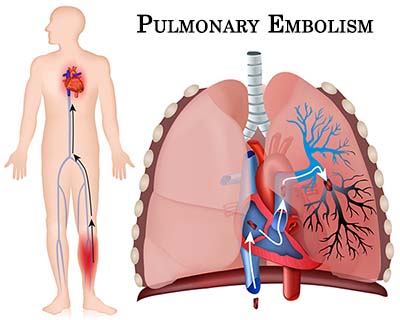
Venous thromboembolic conditions leading to acute respiratory failure is common in critically ill medical and surgical patients. This may be the presenting diagnosis on ICU admission or may develop secondarily in patient admitted to ICU for other conditions. PE presentation is variable presenting suddenly as a cardio respiratory arrest or may be asymptomatic. Mortality can be reduced by prompt diagnosis and therapy . Despite significant advances in the prevention and treatment of VTE, pulmonary embolism remains the most common preventable cause of hospital death, being responsible for approximately 150,000 to 200,000 deaths per year in the United States.
Ministry of Health and Family Welfare has come out with the Standard Treatment Guidelines for Acute Pulmonary Embolism (PE). Following are its major recommendations.
Case definition:
For both situations of care (mentioned below*)
PE refers to obstruction to main pulmonary artery or one of its branches by material (e.g., thrombus, tumor, air, or fat) that originated elsewhere in the body. This topic review focuses on PE due to thrombus. PE can be classified as acute or chronic. Patients with acute PE typically develop symptoms and signs immediately after obstruction of pulmonary vessels. In contrast, patients with chronic PE tend to develop slowly progressive dyspnea over a period of years due to pulmonary hypertension.
Incidence of The Condition In Our Country
The incidence of DVT in India as reported is one percent of the adult population after the age of forty and is 15% to 20% in hospitalized patients. The risk of DVT is 50% in patients undergoing orthopedic surgery, particularly involving the hip and knee, and it is 40% in patients undergoing abdominal or thoracic surgery. 1/100 who developed DVT can develop PE which can be fatal. As per India-specific ENDORSE data presented at Geneva, 1 of 2 hospitalized patients in India is at high risk of developing VTE at any point in time.
- An autopsy data from PGI Chandigarh, where 1,000 consecutive autopsies were performed between 1997 and 2002. 14.4% showed evidence of pulmonary thromboembolism (PTE). 1.45 % of all hospital deaths were due to PTE
- The mean age was 37 years with a male preponderance in the ratio of 1.82:1
- Clinical suspicion was present in 29.17 % of cases
- The most common underlying cases were
o Sepsis (40.28%) o Respiratory illness (10.42%)
o Malignancies (9.72%) o Renal disease (8.3%)
o Hepatobiliary disease (7.64%)
o Cardiovascular disorder (6.94%)
o Gastrointestinal tract disorder (3.47%)
o Vasculitis (2.78%)
Differential Diagnosis / Types
Acute PE can be further classified as massive or sub massive:
- Massive PE causes hypotension, defined as a systolic blood pressure <90 mmHg or a drop in systolic blood pressure of ≥40 mmHg from baseline for a period >15 minutes. It should be suspected anytime there is hypotension accompanied by an elevated central venous pressure (or neck vein distension), which is not otherwise explained by acute myocardial infarction, tension pneumothorax, pericardial tamponade, or a new arrhythmia.
- All acute PE not meeting the definition of massive PE are considered submassive PE.
- A saddle PE is a PE that lodges at the bifurcation of the main pulmonary artery into the right and left pulmonary arteries. Most saddle PE are submassive.
- Acute PE should be differentiated from other causes of acute breathlessness
o Pneumonia
o Pneumothorax
o Acute Left Ventricular failure
o Acute exacerbation of COPD
o Acute bronchial asthma
Pevention And Counseling
Most of the acute PEs originate from deep venous thrombosis (DVT) of legs. Assessing patients at risk for DVT and preventing its occurrence decreases the incidence of acute PE
Assess the risk factors for PE and deep venous thrombosis (DVT) from past medical history as mentioned below:
- Prior venous thromboembolism.
- Immobility for more than 48 hours—congestive heart failure, septic shock, surgery with general anesthesia, on mechanical ventilation.
- Abdominal or lower extremity surgery or trauma.
- Hypercoagulable states.
- Malignancy.
- Spinal cord injury.
- Heparin-induced thrombocytopenia.
- Pregnancy or use of oral contraceptives.
- Indwelling central venous catheters
- Obesity
- Congestive heart failure
Initiate adequate DVT prophylaxis
- Unfractionated heparin(UFH) 5,000 I.U. twice or thrice daily subcutaneously.
- Fractionated Low molecular weight heparin – enoxaparin 40 mg sub cut once daily or equivalent
- Fondaparinaux
- In patients with high risk of bleeding mechanical methods like intermittent pneumatic compression or graduated stockings may be tried.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
i) Clinical Diagnosis:
- PE should be suspected in all patients who present with new or worsening dyspnea, chest pain, or sustained hypotension without any other obvious cause
- ASSESS CLINICAL PROBABILITY OF PE: Clinical probability of PE is based on either clinical judgment or clinical decision rules (Wells and Revised Geneva Score) mentioned below.
Therevised Geneva score:
- Heart rate
- Hemoptysis(2 points)
- Unilateral lower limb pain (3 points)
- Active malignant condition (2 points)
- Surgery or fracture within 1 month (2 points)
- Previous deep venous thrombosis or pulmonary embolism (3 points)
- Age older than 65 years (1 point)
- 75 to 94 beats/min (3 points) or
- 95 beats/min or more (5 points)
- Pain on lower-limb deep venous palpation and unilateral edema (4 Points)
The probability is assessed as follows:
Heart rate Low-probability (0 to 3 points)
Intermediate-probability (4 to 10 points)
High-probability (> or =11 points)
Investigations:
- ECG, XRAY CHEST (PA view) and ABG should be ordered in all these patients. Although these tests are nonspecific they do increase the index of suspicion.
Treatment:
- Provide oxygen to maintain saturation at more than 90%
- If the patient is hypotensive, administer 500 to 1000 ml isotonic crystalloid. Any more volume resuscitation should be given with caution as it may increase RV wall tension and cause ischemia and worsening of shock.
- While diagnostic confirmation is awaited, anticoagulant treatment withsubcutaneouslow molecular weight heparin or intravenousunfractionated (UFH) heparin should be initiated as soon as possible in patients with a high clinical probability of PE if there are no contraindications.
- UFH is preferred in hemodynamically unstable patients in whom thrombolytic therapy is being planned. UFH is also preferred in critically ill patients in the ICU with PE requiring numerous procedures. It is also preferred in patients with renal failure. Patients are considered to be hemodynamically unstable if they are in shock or have a systolic blood pressure of less than 90 mm Hg or a drop in systolic pressure of more than 40 mm Hg for more than 15 minutes in the absence of new onset arrhythmia, hypovolemia, or sepsis
Most patients with acute PE are candidates for initial anticoagulant treatment with subcutaneous lowmolecular-weight heparin or fondaparinux or intravenous UFH. LMWH and Fondaparinux are preferred over UFH.
The usual doses of Anticoagulation for PE are:
1) UFH: Bolus of 80units IV/kg or 5000 IU followed by infusion at 18 units IU /kg/hr. Keeping APTT between 1.5 and 2.5 to normal.
2) Weight based normogram of heparin infusion
3) Fondaparinux:
- Weight < 50kg - 5mg s/c once a day.
- Weight 50-100kg - 7.5mg s/c once a day
- Weight >100 kg – 10mg s/c once a day.
4) Enoxaparin: 1 mg /kg s/c twice a day.
Referral criteria:
- All patients with massive PE should be referred to a higher centre
The risk of adverse outcome is also more in the following situations and these patients should be referred :
o Shock (SBP < 90mmof Hg) and/or BP drop >= 40mm of Hg for >15min and sustained hypotension.
o Immobilization due to neurological disease.
o Age 75 years or more.
o Cardiac, renal or respiratory disease or cancer
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis:
- PE should be suspected in all patients who present with new or worsening dyspnea, chest pain, or sustained hypotension without any other obvious cause
- ASSESS CLINICAL PROBABILITY OF PE: Clinical probability of PE is based on either clinical judgment or clinical decision rules (Wells and Revised Geneva Score) mentioned below.
Therevised Geneva score:
- Heart rate
- Hemoptysis(2 points)
- Unilateral lower limb pain (3 points)
- Active malignant condition (2 points)
- Surgery or fracture within 1 month (2 points)
- Previous deep venous thrombosis or pulmonary embolism (3 points)
- Age older than 65 years (1 point)
- 75 to 94 beats/min (3 points) or
- 95 beats/min or more (5 points)
- Pain on lower-limb deep venous palpation and unilateral edema (4 Points)
The probability is assessed as follows:
Heart rate Low-probability (0 to 3 points)
Intermediate-probability (4 to 10 points)
High-probability (> or =11 points)
Investigations:
If the patient has a high probability of PE clinically or on the basis of a high probability score, and is safely transferable to CT room and is in a position to cooperate with breath holding, he should undergo multidetector CT (MDCT) for CT Pulmonary Angiography irrespective of his hemodynamic status.
If the patient is hemodynamically unstable and has a high probability of PE clinically or on the basis of a high probability score and who is critically ill and can not be shifted, he should be subjected to Trans-esophageal Echo (TEE,), lower extremity ultrasonography and his blood sample sent for a D- Dimer level. A negative Echo and Venous Doppler, however, do not rule out clinically significant PE.Efforts should be made to stabilize this patient hemodynamically and once the patient stabilizes, he should be sent for MDCT CT Pulmonary Angiography, if doubt still remains about the diagnosis.
If the patient is hemodynamically stable and has a low or medium probability score then order a high sensitivity D- Dimer level (ELISA). If it is positive (level more than 500ng/ml) further testing with CT chest is indicated.
If it is negative the risk of PTE is very low (0.14%) and no further testing is required.
A V/Q scan may be done in patients with a high probability of PE and where there is a contraindication for CT like renal failure or if CT scanning is not available.
In pregnant women with clinical findings suggestive of PE, an MDCTchest should be done. The concern about radiation is overcome by the hazard of missing a potentially fatal diagnosis or exposing the mother and fetus to unnecessary anticoagulant treatment. Multidetector CT delivers a higher dose of radiation to the mother but a lower dose to the fetus than V/Q scanning. Venous ultrasonography can be done in these patients before MDCT. j)
Treatment:
Consider Thrombolysis :
a) If the patient is hemodynamically unstable:
i. Admit in ICU
ii. Start anticoagulation, preferably IV unfractionated heparin or LMWH. Keep APTT time 1.5-2.5 to normal.
iii. Administer thrombolytic therapy if there are no contraindications (Table1).
iv. Other supportive measure to stabilize the patient.
b) Hemodynamically
stable patients with right myocardial dysfunction and injury suggested by TEE and markers (raised Troponin and BNP) can also be given thrombolytic therapy if there are no contraindications (Table 2).
Consider Surgical Treatment
Table 1
| Thrombolytic therapy regimens for acute pulmonary embolism |
| Drug | Protocol |
| Streptokinase | 250,000 U IV (loading does during 30 mins; then 100,000 U/h for 24 hours |
| Urokinasea | 250,000 U IV (loading does during 10 mins; then 2,000 U/lb/h for 12 to 24 hours |
| IV, intravenous; tPA, tissue-type plasminogen activator. 100 mg IV during 2h |
Hemodynamically stable patient with PE without myocardial dysfunction or injury:
Admit in ward.
Anti-coagulate with LMWH or Fondaparinux or UFH.
Closely watch for vitals and respiratory distress. Consider early mobilization.
Table2
Contraindication for thrombolytic therapy:
Absolute contraindications
- Prior intracranial hemorrhage (ICH)
- Known structural cerebral vascular lesion Known malignant intracranial neoplasm
- Ischemic stroke within 3 months
- Suspected aortic dissection
- Active bleeding or bleeding diathesis (excluding menses) significant closed-head trauma or facial trauma within 3 months
Relative contraindications
- History of chronic, severe, poorly controlled hypertension
- Severe uncontrolled hypertension on presentation (SBP >180 mm Hg or DBP >110 mm Hg)
- Traumatic or prolonged (>10 min) CPR or major surgery less than 3 weeks
- Recent (within 2-4 wk) internal bleeding
- Non compressible vascular punctures
- For streptokinase/anistreplase - Prior exposure (more than 5 d ago) or prior allergic reaction to these agents
- Pregnancy
- Active peptic ulcer
- Current use of anticoagulant (e.g., warfarin sodium) that has produced an elevated international normalized ratio (INR) >1.7 or prothrombin time (PT) >15 seconds
Initiate Vitamin K Antagonist (Warfarin) Therapy :
- Vitamin K antagonist should be initiated as soon as possible preferably on the first treatment day and Heparin should be continued. Heparin should be discontinued when INR reaches a level of 2.0 or higher for at least 24 hours. Duration of treatment is from 3 to 6 months.
- LMWH is preferred over Warfarin in Cancer and in pregnant women for longterm treatment.
: Inferior vena caval filters are indicated in the following conditions:
- Recurrent thromboembolism despite anticoagulant therapy
- Contraindication to anticoagulation therapy
- Bleeding while on anticoagulants.
Patient should be put on long term anticoagulant treatment in the following conditions:
- Idiopathic pulmonary embolism
- Recurrent PE
- Cancer
Guidelines by The Ministry of Health and Family Welfare :
Rajesh Chawla, Consultant Physician and Intensivist, Indraprastha Apollo Hospital, Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd