- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
ACOG Guidelines on management of intrapartum Intra-amniotic Infection
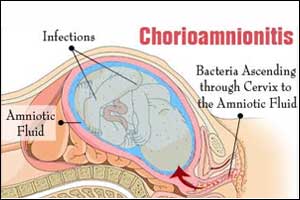
American College of Obstetricians and Gynecologists have released guidelines on the management of intrapartum Intra-amniotic Infection which have been published online in August issue of Obstetrics & Gynecology.Intra-amniotic Infection is usually associated with acute neonatal morbidity, including neonatal pneumonia, meningitis, sepsis, and death.Children who survive may develop long-term complications such as bronchopulmonary dysplasia and cerebral palsy during infancy.
Key Recommendations
- According to the committee opinion, clinicians should suspect intraamniotic infection when the mother's temperature is 39.0°C or higher or when it is between 38.0°C and 38.9°C in the presence of another clinical risk factor such as maternal leukocytosis, purulent cervical drainage, or fetal tachycardia.
- Administration of intrapartum antibiotics and antipyretics is recommended whenever an intra-amniotic infection is suspected or confirmed. Antibiotics should be considered in the setting of isolated maternal fever unless a source other than intra-amniotic infection is identified and documented.
- As intraamniotic infection is usually associated with dysfunctional labor therefore clinicians should ensure labor progresses normally in affected women. Intraamniotic infection alone is not an indication for immediate delivery and is rarely a reason for cesarean delivery.
- Recommended antibiotic regimens for treatment of intraamniotic infection are ampicillin and gentamicin, cefazolin and gentamicin, or clindamycin or vancomycin and gentamicin.
- Antibiotic therapy should only be continued postdelivery in women with risk factors for postpartum endometritis, such as bacteremia or persistent fever
- Clinicians should also consider antibiotic therapy in cases of isolated maternal fever, unless a secondary cause is apparent.
- There is a critical need for clinician communication between the maternal and neonatal healthcare teams.Timely maternal management together with notification of the neonatal health care providers will facilitate appropriate evaluation and empiric antibiotic treatment when indicated.
It is very important that when obstetrician-gynecologists or other obstetric care providers diagnose an intra-amniotic infection, or when other risk factors for early-onset neonatal sepsis are present in labor (eg, maternal fever, prolonged rupture of the membranes, or preterm birth), communication with the neonatal care team is essential to optimize neonatal evaluation and management.
For full text or further reference log on to :
Obstet Gynecol. 2017;130(2):e95-e101

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd