- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
AAO-HNSF Updated Clinical Practice Guideline: Adult Sinusitis
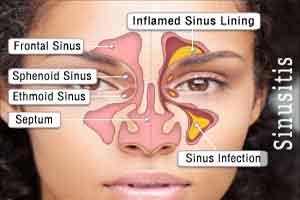
An updated clinical practice guideline from the American Academy of Otolaryngology—Head and Neck Surgery Foundation published in Otolaryngology–Head and Neck Surgery identifies quality improvement opportunities and explicit actionable recommendations for clinicians managing adult sinusitis, including a greater focus on patient education and patient preference.
The differences between the 2007 guideline and the 2015 update include:
- more explicit details about the role of pain relievers, topical intranasal steroids, and/or nasal saline irrigation for symptomatic relief of acute bacterial sinusitis;
- a recommendation of amoxicillin with or without clavulanate when antibiotics are prescribed, while the prior guideline recommended amoxicillin alone;
- several statements about chronic sinusitis, the management of which was not discussed in the 2007 guideline.
Major Recommendations :
1A. Differential Diagnosis Of Acute Rhinosinusitis (ARS): Clinicians should distinguish presumed acute bacterial rhinosinusitis (ABRS) from ARS caused by viral upper respiratory infections and noninfectious conditions. A clinician should diagnose ABRS when(a) symptoms or signs of ARS(purulent nasal drainage accompanied by nasal obstruction, facial pain/pressure/fullness,or both) persist without evidence of improvement for at least 10 days beyond the onset of upper respiratory symptoms or (b) symptoms or signs of ARS worsen within 10 days after an initial improvement (double worsening)
1B. Radiographic Imaging And Acute Rhinosinusitis (ARS): Clinicians should not obtain radiographic imaging for patients who meet diagnostic criteria for ARS, unless a complication or alternative diagnosis is suspected.
2.Symptomatic Relief Of Acute Bacterial Rhinosinusitis(VRS): Clinicians may recommend analgesics, topical intranasal steroids, and/or nasal saline irrigation for symptomatic relief of VRS.
3. Symptomatic Relief Of Acute Bacterial Rhinosinusitis (ABRS): Clinicians may recommend analgesics, topical intranasal steroids,and/or nasal saline irrigation for symptomatic relief of ABRS.
4. Initial Management Of Acute Bacterial Rhinosinusitis (ABRS): Clinicians should either offer watchful waiting (without antibiotics) or prescribe initial antibiotic therapy for adults with uncomplicated ABRS. Watchful waiting should be offered only when there is assurance of follow-up such that antibiotic therapy is started if the patient’s condition fails to improve by 7 days
after ABRS diagnosis or if it worsens at any time.
5. Choice Of Antibiotic For Acute Bacterial Rhinosinusitis (ABRS): If a decision is made to treat ABRS with an antibiotic agent, the clinician should prescribe amoxicillin with or without clavulanate as first-line therapy for 5 to 10 days for most adults.
6. Treatment failure For Acute Bacterial Rhinosinusitis (ABRS): If the patient fails to improve with the initial management option by 7 days after diagnosis or worsens during the initial management, the clinician should reassess the patient to confirm ABRS, exclude other causes of illness, and detect complications. If ABRS is confirmed in the patient initially managed with observation, the clinician should begin antibiotic therapy. If the patient was initially managed with an antibiotic, the clinician should change the antibiotic.
7A. Diagnosis Of Chronic Rhinosinusitis (CRS) Or Recurrent Acute Rhinosinusitis (ARS): Clinicians should distinguish CRS and recurrent ARS from isolated episodes of acute bacterial rhinosinusitis (ABRS) and other causes of sinonasal symptoms.
7B. Objective Confirmation Of Adiagnosis Of Chronic Rhinosinusitis (CRS): The clinician should confirm a clinical diagnosis of CRS with objective documentation of sinonasal inflammation, which may be accomplished using anterior rhinoscopy, nasal endoscopy, or computed tomography.
8. Modifying factors: Clinicians should assess the patient with chronic rhinosinusitis (CRS) or recurrent acute rhinosinusitis (ARS) for multiple chronic conditions that would modify management, such as asthma, cystic fibrosis, immunocompromised state, and ciliary dyskinesia.
9. Testing For Allergy And Immune Function: The clinician may obtain testing for allergy and immune function in evaluating a patient with chronic rhinosinusitis (CRS) or recurrent acute rhinosinusitis (ARS).
10. Chronic Rhinosinusitis (CRS) With Polyps: The clinician should confirm the presence or absence of nasal polyps in a patient with CRS.
11. Topical Intranasal Therapy For Chronic Rhinosinusitis (CRS): Clinicians should recommend saline nasal irrigation, topical intranasal corticosteroids, or both for symptom relief of CRS.
12. Antifungal Therapy For Chronic Rhinosinusitis (CRS): Clinicians should not prescribe topical or systemic antifungal therapy for patients with CRS.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd