- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
A Case of Levamisole induced Agranulocytosis
Levamisole is a broad-spectrum antihelminthic which is used currently in veterinary medicine. In humans, the drug was found to have immune-stimulant and anti-inflammatory properties and has been used for the treatment of rheumatoid arthritis, nephrotic syndrome, and other autoimmune diseases.
A case of Levamisole-Cocaine-Induced Agranulocytosis has been reported by Dr.Thamer Kassim from Department of Internal Medicine, Creighton University, Omaha, NE, USA and associates which has appeared in the journal Case Reports in Hematology.
A sixty-eight-year-old male presented to the Emergency Department (ED) complaining of recurrent diarrhea and a documented fever of 312 K for a one-day duration. The patient had a past medical history of end-stage renal disease on hemodialysis, insulin-dependent type II diabetes mellitus, essential hypertension, and chronic cocaine dependence. On further history, the patient reported the use of cocaine over the past five years with an average use of three times a week but could not specify a certain amount on each time. The patient disclosed that he had used cocaine earlier that day.
At admission, blood pressure was 106/78, heart rate was 96 beats per minute, respiratory rate was 18, the temperature was 312.2 K, and oxygen saturation was 93% on room air. Physical examination showed a thin, malnourished male with right below knee amputation who was in mild distress. No cutaneous manifestations were noticed, and no other abnormalities were appreciated on the rest of the patient's physical examination.
Laboratory workup was done and included a complete blood count (CBC) with differential, which showed a WBC count of 1.9 × 109/L (reference range: 4.0–11.0 × 109/L), segmented neutrophils 4% (reference range: 40–70%), bands 1% (reference range: 0–6%), immature granulocytes of 0.0% (reference range: 0.0–0.9%), and lymphocytes 70% (reference range: 16–45%). Basophils, eosinophils, and monocytes were within normal limits. Hemoglobin was 9.8 g/dL (reference range: 12.5–17 g/dL), which was around the baseline and was attributed to the patient's end-stage renal disease, and platelet count was 237 × 109/L (reference range: 150–450 × 109/L). A complete metabolic profile was also obtained showing a serum potassium of 3.1 mmol/L (reference range: 3.6–5.0 mmol/L), creatinine of 371.4 µmol/L (reference range: 45–90 µmol/L), blood urea nitrogen of 9.64 mmol/L (reference range: 2.5–7.1 mmol/L), and glomerular filtration rate of 12 with a normal liver function.
Urine drug screen was positive for cocaine. Erythrocyte sedimentation rate, C-reactive protein, and urine analysis were within reference range. At that point, isoantibodies including cytoplasmic antineutrophil cytoplasmic antibody (C-ANCA) and perinuclear antineutrophil cytoplasmic antibody (P-ANCA) were not tested because the patient had normal inflammatory markers and no urinary, pulmonary, or cutaneous manifestations.
The patient was admitted to the hospital, and intravenous fluids were initiated along with correction of electrolyte disturbances and symptomatic therapy. The patient's diarrhea resolved during his first admission day, but the patient spiked a fever with a temperature maximum of 313.6 K. A repeat CBC with differential was done and showed a WBC count of 1.0 × 109/L, segmented neutrophils of 3%, bands of 1%, immature granulocytes of 0.0%, and lymphocytes of 44% with normal basophils, eosinophils, and monocytes. The patient's calculated ANC was 40 cells/mm3, and the decision to start empirical antibiotics and initiate a septic workup was taken. Blood cultures, urine analysis and culture, and stool analysis and culture were all negative. Chest X-ray and chest/abdomen CT scan showed no abnormalities, and ultimately no source of infection was isolated.
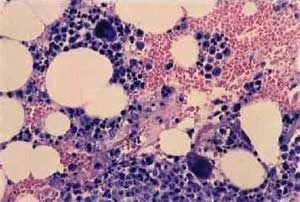
Further tests were initiated in an attempt to find a cause for the patient's unexplained neutropenia. Medications were reviewed carefully for possible idiosyncratic drug reactions and bone marrow toxicity, but none of the patient's medications fit such a profile. A viral panel including hepatitis A, B, and C and HIV were all negative. Vitamin B12 level was 681.7 pmol/L (reference range: 216–687 pmol/), folate level was 38.7 nmol/L (reference range: 4.5–45.3 nmol/L), copper level of 11.2 µmoI/L (reference range: 9.9–23.1 µmoI/L), reticulocyte count of 2.3% (reference range: 0.5–2.3%), lactate dehydrogenase level of 380 IU/L (reference range: 313–680 IU/L), and negative antinuclear antibody test. A peripheral smear showed a decreased number of morphologically unremarkable neutrophils in the background of anemia. The patient refused a bone marrow biopsy.
On the fourth hospital admission day, the patient started to recover on empirical antibiotics and supportive care. The thought of an adulterant in cocaine was brought up as the patient's WBC started to improve after abstinence from drug use. Blood and urine testing for levamisole were not performed due to the short half-life of the drug and the fact that it would not have been detected at that point.
Given the patient's clinical picture, laboratory findings, and no alternative cause of his agranulocytosis, the diagnosis of levamisole-cocaine-induced neutropenia was thought to be most appropriate as a diagnosis of exclusion. The patient's white blood cell count and absolute neutrophil count started to recover four to five days after stopping cocaine use which suggested an association.
It also showed to be beneficial in the management of lung, colon, and breast cancer.
For more reference log on to https://doi.org/10.1155/2018/7341835

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd