- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
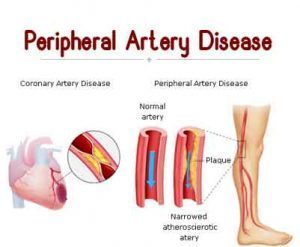
Peripheral Arterial Disease-Standard Treatment Guidelines
Introduction
The term “Peripheral Arterial Disease (PAD)” broadly encompasses the vascular diseases caused primarily by atherosclerosis and thromboembolic pathophysiological processes that alter the normal structure and function of the aorta, iliac and the arteries of the lower extremity. Patients with PAD have an increased risk of mortality, myocardial infarction, and cerebrovascular disease. They also suffer from significant functional limitations in their daily activities, and the most severely affected are at risk of limb loss.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Peripheral Arterial Disease.
Following are the major recommendations :
Case definition
Peripheral arterial disease (PAD) is the preferred clinical term that should be used to denote stenotic and occlusive diseases of the aorta and its branch arteries, exclusive of the coronary arteries.
Incidence of the condition in our country
It is underdiagnosed, undertreated, and much more common than previously thought. Incidence of the condition in our country is not exactly known due to lack of organized data. A strong association exists between advancing age and the prevalence. Almost 20% of adults older than 70 years have PAD. An American survey of 2174 patients older than 40 years of age used the Ankle-Brachial Index (ABI) as a screening tool, and showed a PAD prevalence of 0.9% between the ages of 40 and 49 years, 2.5% between the ages of 50 and 59 years, 4.7% between the ages of 60 and 69 years, and 14.5% for the ages of 70 years and older(2).
| Differential Diagnosis of Intermittent Claudication | ||||||
| Condition | Location of Pain or Discomfort | Characteristic Discomfort | Onset Relative to Exercise | Effect of Rest | Effect of Body Position | Other Characteris tics |
| Intermittent claudication | Buttock, thigh, or calf muscles and rarely the foot | Cramping, aching, fatigue, weakness, or frank pain | After same degree of exercise | Quickly relieved | None | Reproducible |
| Nerve root compression (e.g., herniated disc) | Radiates down leg, usually posteriorly | Sharp lancinating pain | Soon, if not immediately after onset | Not quickly relieved (also often present at res | Relief may be aided by adjusting back position | History of back problems |
| Spinal stenosis | Hip, thigh, buttocks (follows dermatome) | Motor weakness more prominent than pain | After walking or standing for variable lengths of time | Relieved by stopping only if position changed | Relief by lumbar spine flexion (sitting or stooping forward) | Frequent history of back problems, provoked by intraabdominal pressure |
| Arthritic, inflammatory processes | Foot, arch | Aching pain | After variable degree of exercise | Not quickly relieved (and may be present at rest) | May be relieved by not bearing weight | Variable, may relate to activity level |
| Hip arthritis | Hip, thigh, buttocks | Aching discomfort, usually localized to hip and gluteal region | After variable degree of exercise | Not quickly relieved (and may be present at rest) | More comfortable sitting, weight taken off legs | Variable, may relate to activity level, weather changes |
| Symptomatic Baker’s cyst | Behind knee, down calf | Swelling, soreness, tenderness | With exercise | Present at rest | None | Not intermittent |
| Venous claudication | Entire leg, but usually worse in thigh and groin | Tight, bursting pain | After walking | Subsides slowly | Relief speeded by elevation | History of iliofemoral deep vein thrombosis, signs of venous congestion, edema |
| Chronic compartment syndrome | Calf muscles | Tight, bursting pain | After much exercise (e.g., jogging) | Subsides very slowly | Relief speeded by elevation | Typically occurs in heavy muscled athletes |
Prevention and Counselling
Individuals at risk for lower extremity disease should undergo a vascular review of symptoms to assess walking impairment, claudication, ischemic rest pain and/or the presence of non - healing wounds.
Aggressive lifestyle modification to reduce underlying risk factors (e.g. atherogenic diet, overweight or obesity, physical inactivity), to control risk factors such as diabetes, hypertension and hyperlipidemia are recommended for individuals with asymptomatic lower extremity PAD.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria -
Diagnostic Criteria
PAD is considered in the following clinical setting -
- Adults 50 years and older who have atherosclerosis risk factors and
- Adults 70 years and older with the following symptoms -
- Fatigue, aching, numbness or pain in the lower extremity or any history of walking
impairment (suggesting exertional limitation of the lower extremity muscles). - Pain at rest localized to the lower leg or foot and its association with the upright or recumbent positions.
- Poorly healing or non-healing wounds of the legs or feet.
Acute limb ischemia (ALI) - refers to a rapid decrease of perfusion in the affected extremity that requires urgent revascularization to preserve tissue viability. Complications include rhabdomyolysis and renal failure.
Chronic Limb Ischemia (CLI) - refers to a chronic, severely compromised arterial blood supply in the affected extremity that manifests as ischemic pain at rest, ulcers or gangrene in various combinations.
Investigations
1. Measurement of Ankle-Brachial Index (ABI)
2. Color Doppler evaluation -
Color flow and pulsed wave Doppler allows an estimation of the stenosis severity on the basis of Doppler-derived velocity criteria. It is an accurate method for determining the degree of stenosis or length of occlusion of the arteries supplying the lower extremity. It is also useful in the follow-up of patients who have undergone endovascular (percutaneous transluminal angioplasty/stent) or surgical revascularization.
3. Magnetic Resonance Angiography (MRA) -
Magnetic resonance angiography (MRA) of the aorta and peripheral vasculature can be performed rapidly with excellent image quality. Being noninvasive, it is virtually replacing invasive diagnostic angiography as the primary modality for vascular imaging. Determining the type of intervention is feasible on a technically adequate MRA study. However, availability of the scanners with capability for peripheral vascular imaging and patients with relative contraindications to MR evaluation limits the utilization.
4. Computed Tomographic Angiography (CTA) -
Higher spatial resolution, absence of flow-related phenomena that may distort MRA images and the capacity to visualize calcification and metallic implants such as endovascular stents or stent grafts is an advantage with CTA when compared with MRA. Its advantages over invasive angiography include volumetric acquisition, improved visualization of soft tissues and other adjacent anatomic structures, less invasiveness and thus fewer potential complications. Exposure to ionizing radiation and the need for iodinated contrast medium limits its utilization as also availability of scanners with capability for peripheral vascular imaging.
5. Digital Subtraction Angiography (DSA) -
Vascular imaging with ultrasonography, CTA, and MRA has replaced catheter-based techniques in the initial diagnostic evaluation in most circumstances. The major advantage of DSA is the ability to selectively evaluate individual vessels, obtain physiologic information such as pressure gradients and as a platform for percutaneous intervention. Exposure to ionizing radiation, use of iodinated contrast agents, and risks related to vascular access and catheterization are limitations of this technique.
Treatment
Two major strategies for treatment are:
- To improve symptoms and quality of life with medical therapy alone or with percutaneous / surgical revascularization and
- To prevent cardiovascular events with a comprehensive program that includes smoking cessation, an exercise program, control of blood pressure, achievement of goal LDL-C, antiplatelet therapy, and control of diabetes.
Asymptomatic Lower Extremity PAD -
1. Smoking cessation, lipid lowering, diabetes and hypertension treatment.
2. Antiplatelet therapy - to reduce the risk of adverse cardiovascular ischemic events.
3. Angiotensin-converting enzyme (ACE) inhibition.
Symptomatic Lower extremity PAD-
Medical Management-
Best medical treatment is considered the main therapeutic pillar in patients with PAD. These patients are at increased risk for major adverse cardiovascular events (MACE) and cardiovascular death. Antithrombotic, antihypertensive and lipid lowering therapy has been shown to reduce the relative risk by 25% each. Medication should only be used in combination with aggressive lifestyle modification to reduce underlying lifestyle risk factors as mentioned above.
Revascularization
Before offering revascularization, a predicted or observed lack of adequate response to exercise therapy and claudication pharmacotherapies must be considered. Three clear indications for revascularization in patients with PAD are ischemic rest pain, ischemic ulcers or gangrene, and claudication that interfere with the patient's lifestyle.
Revascularization by endovascular or surgical means, will be guided by the lesion morphology based on TASC II (Trans Atlantic Society Consensus) document criteria, where TASC A & B lesions are treated by endovascular approach and type D lesion are treated surgically. TASC C lesions can be attempted by endovascular approach and if the same fails, surgery is resorted to.
Endovascular procedures for revascularization depend upon whether the clinical presentation is acute or chronic and whether it is because of thrombotic occlusion or steno-occlusive lesion. Acute thrombotic occlusions are treated by Catheter directed thrombolysis, whereas chronic occlusions may require mechanical thrombectomy. Stenosis and short length occlusions (TASC A & B) are treated by Angioplasty & Stenting. Diffuse atheromatous plaques causing stenosis require Plaque Excisional Atherectomy. Long length occlusions in Iliac and SFA may yield to subintimal angioplasty followed by stent insertion if needed.
Referral Criteria
Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited:
Clinical Diagnosis: Same diagnostic criteria as above.
Investigations: Following thorough clinical evaluation, following investigations are required -
- Measurement of Ankle-Brachial Index (ABI) & hand held vascular doppler.
- Color Doppler Sonography.
- Magnetic Resonance Angiography (MRA) or Computed Tomographic Angiography (CTA).
Treatment:
Asymptomatic Lower Extremity PAD - Smoking cessation, lipid lowering, diabetes and hypertension treatment. Antiplatelet therapy - to reduce the risk of adverse cardiovascular ischemic events (10, 11).
Symptomatic Lower extremity PAD – Best medical treatment is considered the main therapeutic pillar in patients with PAD. These patients are at increased risk for major adverse cardiovascular events (MACE).
Symptomatic Lower extremity PAD:
- Modification of lifestyle to improve diet and physical activity and to control obesity,
diabetes, hypertension and hyperlipidemia. - Medical treatment with antithrombotic, antihypertensive and lipid lowering drugs.
- Revascularization, either endovascular or surgical (12).
Standard Operating Procedure
Out Patient / Day Care – Asymptomatic and symptomatic patients with less severe symptoms are treated on an Outpatient or Day Care basis.
Referral criteria:Patients may be referred to higher medical facility based upon -
- Worsening of symptoms despite adequate medical management including aggressive lifestyle modification.
- Patient presents with acute limb ischemia (ALI) where immediate limb salvage is required.
Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis: Same diagnostic criteria as above.
Investigations:
1. Measurement of Ankle-Brachial Index (ABI) & hand held vascular doppler
2. Color Doppler Sonography
3. Magnetic Resonance Angiography (MRA) or
4. Computed Tomographic Angiography (CTA)
5. Digital Subtraction Angiography (DSA)
Treatment:
Asymptomatic Lower Extremity PAD-
1. Smoking cessation, lipid lowering, diabetes and hypertension treatment.
2. Antiplatelet therapy - to reduce the risk of adverse cardiovascular ischemic events.
Symptomatic Lower extremity PAD-
1. Aggressive lifestyle modification to reduce underlying lifestyle risk factors (e.g. atherogenic diet, overweight/obesity, physical inactivity) to control risk factors such as diabetes, hypertension and hyperlipidemia.
2. Medical treatment with antithrombotic, antihypertensive and lipid lowering therapy is given to reduce the relative risk of adverse events.
3. Revascularization – endovascular or surgical.
Standard Operating procedure
a) Out Patient - Asymptomatic and symptomatic patients with less severe symptoms are treated on an Outpatient or Day Care basis.
b) In Patient - Symptomatic patients requiring revascularization will need hospitalization for minimum duration depending upon endovascular or surgical approach, where the former approach requires shorter hospital stay. Similarly patients with major adverse cardiovascular events will need hospitalization to treat the adverse events.
Referral Criteria:
Worsening of symptoms despite adequate medical management including aggressive lifestyle modification or patient presents with acute limb ischemia where immediate limb salvage is required.
| Designation | Clinical Role | Timeline | ||
| Physician (Internist) | Clinical Evaluation | Screening on presentation to OP | ||
| Vascular Surgeon (VS) | Clinical Evaluation & supervising vascular evaluation | Specialist Consultant who becomes the primary care Physician once diagnosis is established | ||
| Performs Vascular Surgery | When indicated or when IR procedures fail. | |||
| Biochemist | Biochemical evaluation | After evaluation by and on the request of VS | ||
| Diagnostic Radiologist | Perform Duplex Doppler Sonography, Evaluate CTA or MRA | After evaluation by and on the request of VS | ||
| Cardiologist | Cardiac evaluation | After consultation by and on the request of VS | ||
| Management of MACE | If necessary, following VS consult and on the request of VS | |||
| Interventional Radiologist | IR Procedures – PTRA & Stenting, Thrombolysis, Mechanical thrombectomy, Subintimal Angioplasty etc. | Referring Specialist for IR procedures on the request of VS | ||
| Nursing Staff | Assist in managing the patient | In-patient or Day Care in Vascular Surgery facility, Dialysis facility and Interventional Radiology facility | ||
| Technician | Assist in Imaging the patient | In CT,MR and Interventional Radiology facility after Radiology & IR consultation | ||
RESOURCES REQUIRED FOR ONE PATIENT / PROCEDURE (PATIENT WEIGHT 60 KGS)
(Units to be specified for human resources, investigations, drugs & consumables and equipment. Quantity to also be specified)
| SITUATION | HUMAN RESOURCES | INVESTIGATIONS | DRUGS & CONSUMABLES | EQUIPMENT |
| 1. | Doctors – (Internist – 1, Vascular Surgeon – 1, Diagnostic Radiologist -1, Technician(s) – 3, Nursing - 2 | Hemoglobin, Random Blood Sugar, PT, APTT or INR, Platelet Count, Se. Creatinine, HBsAg, HIV | 1. Drugs: Aspirin, Clopidogrel, Nitroglycerine, Nimodipine, Heparin | Vascular Doppler(1) Color Doppler Ultrasound (1) MDCT or MRI with facility for Vascular Imaging (1) |
| 2. | Doctors – (Internist – 1, Vascular Surgeon with – 1, Diagnostic Radiologist -1, Interventional Radiologist – 1, Anaesthetist -1) Technician(s) – 3 to 4 Nurses – 3 to 4 for all the units | Hemoglobin, Random Blood Sugar, PT, APTT or INR, Platelet Count, Se. Creatinine, HBsAg, HIV | 1. Drugs: Aspirin, Clopidogrel, Nitroglycerine, Nimodipine, Heparin, Non Ionic radiographic contrast media 2. Consumables: Arterial access device, Diagnostic Catheter, Guiding catheter, Self expanding or balloon expanding Stent, Pre and post dilatation angioplasty balloon(s), Compatible guidewire (s) | Vascular Doppler(1) Operation Theatre (1) Color Doppler Ultrasound (1) MDCT or MRI with Vascular Imaging (1) Digital Subtraction Angiography System (1) Sterile Suite Multichannel invasive monitor(1) Resuscitation equipment (1) Crash Trolley (1) |
Guidelines by The Ministry of Health and Family Welfare :
Dr. Chander Mohan
Dr. B.L. Kapur Hospital
New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd